First immunotherapy regimen before and
after surgery to extend survival in bladder cancer
Positive high-level results from the NIAGARA Phase III trial
showed AstraZeneca’s IMFINZI® (durvalumab) in combination with
chemotherapy demonstrated a statistically significant and
clinically meaningful improvement in the primary endpoint of
event-free survival (EFS) and the key secondary endpoint of overall
survival (OS) versus neoadjuvant chemotherapy for patients with
muscle-invasive bladder cancer (MIBC). Patients were treated with
IMFINZI in combination with neoadjuvant chemotherapy before
cystectomy (surgery to remove the bladder) followed by IMFINZI as
adjuvant monotherapy.
Approximately one in four patients with bladder cancer has
evidence of the tumor invading the muscle wall of the bladder
(without distant metastases), known as MIBC.1,2 In the MIBC
setting, approximately 117,000 patients are treated with current
standard of care.3 Standard treatment includes neoadjuvant
chemotherapy and radical cystectomy.4 However, even after
cystectomy, patients experience high rates of recurrence and a poor
prognosis.4
Professor Thomas Powles, MD, Professor, Director of Barts Cancer
Centre (QMUL), London, UK, and investigator in the trial, said:
“Nearly half of patients with muscle-invasive bladder cancer who
receive standard of care still experience disease recurrence or
progression. These NIAGARA data show for the first time that adding
durvalumab to chemotherapy before surgery followed by durvalumab
extends patients’ lives.”
Susan Galbraith, Executive Vice President, Oncology R&D,
AstraZeneca, said: “The NIAGARA results support our strategy to
move immunotherapy to the early stages of cancer treatment. This
perioperative regimen with IMFINZI improved survival and reduced
the rate at which patients experience disease recurrence or
progression. We are eager to bring this regimen with the potential
to transform the standard of care to patients as soon as
possible.”
IMFINZI was generally well-tolerated and no new safety concerns
were observed in either the neoadjuvant or adjuvant setting. The
safety profile of IMFINZI and neoadjuvant chemotherapy was
consistent with the known profile of the individual medicines. The
addition of IMFINZI did not increase the discontinuation rate due
to adverse events and did not compromise patients' ability to
complete surgery compared to neoadjuvant chemotherapy alone. These
data will be presented at a forthcoming medical meeting and shared
with global regulatory authorities.
IMPORTANT SAFETY INFORMATION
There are no contraindications for IMFINZI® (durvalumab) or
IMJUDO® (tremelimumab-actl).
Severe and Fatal Immune-Mediated Adverse Reactions
Important immune-mediated adverse reactions listed under
Warnings and Precautions may not include all possible severe and
fatal immune-mediated reactions. Immune-mediated adverse reactions,
which may be severe or fatal, can occur in any organ system or
tissue. Immune-mediated adverse reactions can occur at any time
after starting treatment or after discontinuation. Monitor patients
closely for symptoms and signs that may be clinical manifestations
of underlying immune-mediated adverse reactions. Evaluate clinical
chemistries including liver enzymes, creatinine,
adrenocorticotropic hormone (ACTH) level, and thyroid function at
baseline and before each dose. In cases of suspected
immune-mediated adverse reactions, initiate appropriate workup to
exclude alternative etiologies, including infection. Institute
medical management promptly, including specialty consultation as
appropriate. Withhold or permanently discontinue IMFINZI and IMJUDO
depending on severity. See USPI Dosing and Administration for
specific details. In general, if IMFINZI and IMJUDO requires
interruption or discontinuation, administer systemic corticosteroid
therapy (1 mg to 2 mg/kg/day prednisone or equivalent) until
improvement to Grade 1 or less. Upon improvement to Grade 1 or
less, initiate corticosteroid taper and continue to taper over at
least 1 month. Consider administration of other systemic
immunosuppressants in patients whose immune-mediated adverse
reactions are not controlled with corticosteroid therapy.
Immune-Mediated
Pneumonitis
IMFINZI and IMJUDO can cause immune-mediated pneumonitis, which
may be fatal. The incidence of pneumonitis is higher in patients
who have received prior thoracic radiation.
- IMFINZI as a Single Agent
- In patients who did not receive recent prior radiation, the
incidence of immune-mediated pneumonitis was 2.4% (34/1414),
including fatal (<0.1%), and Grade 3-4 (0.4%) adverse reactions.
In patients who received recent prior radiation, the incidence of
pneumonitis (including radiation pneumonitis) in patients with
unresectable Stage III NSCLC following definitive chemoradiation
within 42 days prior to initiation of IMFINZI in PACIFIC was 18.3%
(87/475) in patients receiving IMFINZI and 12.8% (30/234) in
patients receiving placebo. Of the patients who received IMFINZI
(475), 1.1% were fatal and 2.7% were Grade 3 adverse
reactions.
- The frequency and severity of immune-mediated pneumonitis in
patients who did not receive definitive chemoradiation prior to
IMFINZI were similar in patients who received IMFINZI as a single
agent or with ES-SCLC or BTC when given in combination with
chemotherapy.
- IMFINZI with IMJUDO
- Immune‑mediated pneumonitis occurred in 1.3% (5/388) of
patients receiving IMFINZI and IMJUDO, including fatal (0.3%) and
Grade 3 (0.2%) adverse reactions.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated pneumonitis occurred in 3.5% (21/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including fatal (0.5%), and Grade 3
(1%) adverse reactions.
Immune-Mediated Colitis
IMFINZI with IMJUDO and platinum-based chemotherapy can cause
immune-mediated colitis, which may be fatal.
IMFINZI and IMJUDO can cause immune-mediated colitis that is
frequently associated with diarrhea. Cytomegalovirus (CMV)
infection/reactivation has been reported in patients with
corticosteroid-refractory immune-mediated colitis. In cases of
corticosteroid-refractory colitis, consider repeating infectious
workup to exclude alternative etiologies.
- IMFINZI as a Single Agent
- Immune-mediated colitis occurred in 2% (37/1889) of patients
receiving IMFINZI, including Grade 4 (<0.1%) and Grade 3 (0.4%)
adverse reactions.
- IMFINZI with IMJUDO
- Immune‑mediated colitis or diarrhea occurred in 6% (23/388) of
patients receiving IMFINZI and IMJUDO, including Grade 3 (3.6%)
adverse reactions. Intestinal perforation has been observed in
other studies of IMFINZI and IMJUDO.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated colitis occurred in 6.5% (39/596) of patients
receiving IMFINZI in combination with IMJUDO and platinum-based
chemotherapy including fatal (0.2%) and Grade 3 (2.5%) adverse
reactions. Intestinal perforation and large intestine perforation
were reported in 0.1% of patients.
Immune-Mediated
Hepatitis
IMFINZI and IMJUDO can cause immune-mediated hepatitis, which
may be fatal.
- IMFINZI as a Single Agent
- Immune-mediated hepatitis occurred in 2.8% (52/1889) of
patients receiving IMFINZI, including fatal (0.2%), Grade 4 (0.3%)
and Grade 3 (1.4%) adverse reactions.
- IMFINZI with IMJUDO
- Immune‑mediated hepatitis occurred in 7.5% (29/388) of patients
receiving IMFINZI and IMJUDO, including fatal (0.8%), Grade 4
(0.3%) and Grade 3 (4.1%) adverse reactions.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated hepatitis occurred in 3.9% (23/596) of patients
receiving IMFINZI in combination with IMJUDO and platinum-based
chemotherapy, including fatal (0.3%), Grade 4 (0.5%), and Grade 3
(2%) adverse reactions.
Immune-Mediated
Endocrinopathies
- Adrenal Insufficiency: IMFINZI and IMJUDO can cause
primary or secondary adrenal insufficiency. For Grade 2 or higher
adrenal insufficiency, initiate symptomatic treatment, including
hormone replacement as clinically indicated.
- IMFINZI as a Single Agent
- Immune-mediated adrenal insufficiency occurred in 0.5% (9/1889)
of patients receiving IMFINZI, including Grade 3 (<0.1%) adverse
reactions.
- IMFINZI with IMJUDO
- Immune-mediated adrenal insufficiency occurred in 1.5% (6/388)
of patients receiving IMFINZI and IMJUDO, including Grade 3 (0.3%)
adverse reactions.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated adrenal insufficiency occurred in 2.2% (13/596)
of patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.8%) adverse
reactions.
- Hypophysitis: IMFINZI and IMJUDO can cause
immune-mediated hypophysitis. Hypophysitis can present with acute
symptoms associated with mass effect such as headache, photophobia,
or visual field cuts. Hypophysitis can cause hypopituitarism.
Initiate symptomatic treatment including hormone replacement as
clinically indicated.
- IMFINZI as a Single Agent
- Grade 3 hypophysitis/hypopituitarism occurred in <0.1%
(1/1889) of patients who received IMFINZI.
- IMFINZI with IMJUDO
- Immune-mediated hypophysitis/hypopituitarism occurred in 1%
(4/388) of patients receiving IMFINZI and IMJUDO.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated hypophysitis occurred in 1.3% (8/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.5%) adverse
reactions.
- Thyroid Disorders (Thyroiditis, Hyperthyroidism, and
Hypothyroidism): IMFINZI and IMJUDO can cause immune-mediated
thyroid disorders. Thyroiditis can present with or without
endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate
hormone replacement therapy for hypothyroidism or institute medical
management of hyperthyroidism as clinically indicated.
- IMFINZI as a Single Agent
- Immune-mediated thyroiditis occurred in 0.5% (9/1889) of
patients receiving IMFINZI, including Grade 3 (<0.1%) adverse
reactions.
- Immune-mediated hyperthyroidism occurred in 2.1% (39/1889) of
patients receiving IMFINZI.
- Immune-mediated hypothyroidism occurred in 8.3% (156/1889) of
patients receiving IMFINZI, including Grade 3 (<0.1%) adverse
reactions.
- IMFINZI with IMJUDO
- Immune-mediated thyroiditis occurred in 1.5% (6/388) of
patients receiving IMFINZI and IMJUDO.
- Immune-mediated hyperthyroidism occurred in 4.6% (18/388) of
patients receiving IMFINZI and IMJUDO, including Grade 3 (0.3%)
adverse reactions.
- Immune-mediated hypothyroidism occurred in 11% (42/388) of
patients receiving IMFINZI and IMJUDO.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated thyroiditis occurred in 1.2% (7/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy.
- Immune-mediated hyperthyroidism occurred in 5% (30/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.2%) adverse
reactions.
- Immune-mediated hypothyroidism occurred in 8.6% (51/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.5%) adverse
reactions.
- IMFINZI with Carboplatin and Paclitaxel
- Immune-mediated hypothyroidism occurred in 14% (34/235) of
patients receiving IMFINZI in combination with carboplatin and
paclitaxel.
- Type 1 Diabetes Mellitus, which can present with diabetic
ketoacidosis: Monitor patients for hyperglycemia or other signs
and symptoms of diabetes. Initiate treatment with insulin as
clinically indicated.
- IMFINZI as a Single Agent
- Grade 3 immune-mediated Type 1 diabetes mellitus occurred in
<0.1% (1/1889) of patients receiving IMFINZI.
- IMFINZI with IMJUDO
- Two patients (0.5%, 2/388) had events of hyperglycemia
requiring insulin therapy that had not resolved at last
follow-up.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated Type 1 diabetes mellitus occurred in 0.5%
(3/596) of patients receiving IMFINZI in combination with IMJUDO
and platinum-based chemotherapy including Grade 3 (0.3%) adverse
reactions.
Immune-Mediated Nephritis with Renal
Dysfunction
IMFINZI and IMJUDO can cause immune-mediated nephritis.
- IMFINZI as a Single Agent
- Immune-mediated nephritis occurred in 0.5% (10/1889) of
patients receiving IMFINZI, including Grade 3 (<0.1%) adverse
reactions.
- IMFINZI with IMJUDO
- Immune-mediated nephritis occurred in 1% (4/388) of patients
receiving IMFINZI and IMJUDO, including Grade 3 (0.5%) adverse
reactions.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated nephritis occurred in 0.7% (4/596) of patients
receiving IMFINZI in combination with IMJUDO and platinum-based
chemotherapy, including Grade 3 (0.2%) adverse reactions.
Immune-Mediated Dermatology
Reactions
IMFINZI and IMJUDO can cause immune-mediated rash or dermatitis.
Exfoliative dermatitis, including Stevens-Johnson Syndrome (SJS),
drug rash with eosinophilia and systemic symptoms (DRESS), and
toxic epidermal necrolysis (TEN), has occurred with PD-1/L-1 and
CTLA-4 blocking antibodies. Topical emollients and/or topical
corticosteroids may be adequate to treat mild to moderate
non-exfoliative rashes.
- IMFINZI as a Single Agent
- Immune-mediated rash or dermatitis occurred in 1.8% (34/1889)
of patients receiving IMFINZI, including Grade 3 (0.4%) adverse
reactions.
- IMFINZI with IMJUDO
- Immune-mediated rash or dermatitis occurred in 4.9% (19/388) of
patients receiving IMFINZI and IMJUDO, including Grade 4 (0.3%) and
Grade 3 (1.5%) adverse reactions.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Immune-mediated rash or dermatitis occurred in 7.2% (43/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.3%) adverse
reactions.
Immune-Mediated
Pancreatitis
IMFINZI in combination with IMJUDO can cause immune-mediated
pancreatitis. Immune-mediated pancreatitis occurred in 2.3% (9/388)
of patients receiving IMFINZI and IMJUDO, including Grade 4 (0.3%)
and Grade 3 (1.5%) adverse reactions.
Other Immune-Mediated Adverse
Reactions
The following clinically significant, immune-mediated adverse
reactions occurred at an incidence of less than 1% each in patients
who received IMFINZI and IMJUDO or were reported with the use of
other immune-checkpoint inhibitors.
- Cardiac/vascular: Myocarditis, pericarditis,
vasculitis.
- Nervous system: Meningitis, encephalitis, myelitis and
demyelination, myasthenic syndrome/myasthenia gravis (including
exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune
neuropathy.
- Ocular: Uveitis, iritis, and other ocular inflammatory
toxicities can occur. Some cases can be associated with retinal
detachment. Various grades of visual impairment to include
blindness can occur. If uveitis occurs in combination with other
immune-mediated adverse reactions, consider a
Vogt-Koyanagi-Harada-like syndrome, as this may require treatment
with systemic steroids to reduce the risk of permanent vision
loss.
- Gastrointestinal: Pancreatitis including increases in
serum amylase and lipase levels, gastritis, duodenitis.
- Musculoskeletal and connective tissue disorders:
Myositis/polymyositis, rhabdomyolysis and associated sequelae
including renal failure, arthritis, polymyalgia rheumatic.
- Endocrine: Hypoparathyroidism.
- Other (hematologic/immune): Hemolytic anemia, aplastic
anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenia, solid organ
transplant rejection, other transplant (including corneal graft)
rejection.
Infusion-Related Reactions
IMFINZI and IMJUDO can cause severe or life-threatening
infusion-related reactions. Monitor for signs and symptoms of
infusion-related reactions. Interrupt, slow the rate of, or
permanently discontinue IMFINZI and IMJUDO based on the severity.
See USPI Dosing and Administration for specific details. For Grade
1 or 2 infusion-related reactions, consider using pre-medications
with subsequent doses.
- IMFINZI as a Single Agent
- Infusion-related reactions occurred in 2.2% (42/1889) of
patients receiving IMFINZI, including Grade 3 (0.3%) adverse
reactions.
- IMFINZI with IMJUDO
- Infusion-related reactions occurred in 10 (2.6%) patients
receiving IMFINZI and IMJUDO.
- IMFINZI with IMJUDO and Platinum-Based Chemotherapy
- Infusion-related reactions occurred in 2.9% (17/596) of
patients receiving IMFINZI in combination with IMJUDO and
platinum-based chemotherapy, including Grade 3 (0.3%) adverse
reactions.
Complications of Allogeneic HSCT after IMFINZI
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with a PD-1/L-1 blocking antibody.
Transplant-related complications include hyperacute
graft-versus-host-disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease (VOD) after reduced intensity conditioning,
and steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between PD-1/L-1 blockade and allogeneic HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with a PD-1/L-1 blocking antibody prior to or
after an allogeneic HSCT.
Embryo-Fetal Toxicity
Based on their mechanism of action and data from animal studies,
IMFINZI and IMJUDO can cause fetal harm when administered to a
pregnant woman. Advise pregnant women of the potential risk to a
fetus. In females of reproductive potential, verify pregnancy
status prior to initiating IMFINZI and IMJUDO and advise them to
use effective contraception during treatment with IMFINZI and
IMJUDO and for 3 months after the last dose of IMFINZI and
IMJUDO.
Lactation
There is no information regarding the presence of IMFINZI and
IMJUDO in human milk; however, because of the potential for serious
adverse reactions in breastfed infants from IMFINZI and IMJUDO,
advise women not to breastfeed during treatment and for 3 months
after the last dose.
Adverse Reactions
- In patients with Stage III NSCLC in the PACIFIC study receiving
IMFINZI (n=475), the most common adverse reactions (≥20%) were
cough (40%), fatigue (34%), pneumonitis or radiation pneumonitis
(34%), upper respiratory tract infections (26%), dyspnea (25%), and
rash (23%). The most common Grade 3 or 4 adverse reactions (≥3%)
were pneumonia (7%) and pneumonitis/radiation pneumonitis
(3.4%).
- In patients with Stage III NSCLC in the PACIFIC study receiving
IMFINZI (n=475), discontinuation due to adverse reactions occurred
in 15% of patients in the IMFINZI arm. Serious adverse reactions
occurred in 29% of patients receiving IMFINZI. The most frequent
serious adverse reactions (≥2%) were pneumonitis or radiation
pneumonitis (7%) and pneumonia (6%). Fatal pneumonitis or radiation
pneumonitis and fatal pneumonia occurred in <2% of patients and
were similar across arms.
- In patients with mNSCLC in the POSEIDON study receiving IMFINZI
and IMJUDO plus platinum-based chemotherapy (n=330), the most
common adverse reactions (occurring in ≥20% of patients) were
nausea (42%), fatigue (36%), musculoskeletal pain (29%), decreased
appetite (28%), rash (27%), and diarrhea (22%).
- In patients with mNSCLC in the POSEIDON study receiving IMFINZI
in combination with IMJUDO and platinum-based chemotherapy (n=330),
permanent discontinuation of IMFINZI or IMJUDO due to an adverse
reaction occurred in 17% of patients. Serious adverse reactions
occurred in 44% of patients, with the most frequent serious adverse
reactions reported in at least 2% of patients being pneumonia
(11%), anemia (5%), diarrhea (2.4%), thrombocytopenia (2.4%),
pyrexia (2.4%), and febrile neutropenia (2.1%). Fatal adverse
reactions occurred in a total of 4.2% of patients.
- In patients with extensive-stage SCLC in the CASPIAN study
receiving IMFINZI plus chemotherapy (n=265), the most common
adverse reactions (≥20%) were nausea (34%), fatigue/asthenia (32%),
and alopecia (31%). The most common Grade 3 or 4 adverse reaction
(≥3%) was fatigue/asthenia (3.4%).
- In patients with extensive-stage SCLC in the CASPIAN study
receiving IMFINZI plus chemotherapy (n=265), IMFINZI was
discontinued due to adverse reactions in 7% of the patients
receiving IMFINZI plus chemotherapy. Serious adverse reactions
occurred in 31% of patients receiving IMFINZI plus chemotherapy.
The most frequent serious adverse reactions reported in at least 1%
of patients were febrile neutropenia (4.5%), pneumonia (2.3%),
anemia (1.9%), pancytopenia (1.5%), pneumonitis (1.1%), and COPD
(1.1%). Fatal adverse reactions occurred in 4.9% of patients
receiving IMFINZI plus chemotherapy.
- In patients with locally advanced or metastatic BTC in the
TOPAZ-1 study receiving IMFINZI (n=338), the most common adverse
reactions (occurring in ≥20% of patients) were fatigue (42%),
nausea (40%), constipation (32%), decreased appetite (26%),
abdominal pain (24%), rash (23%), and pyrexia (20%).
- In patients with locally advanced or metastatic BTC in the
TOPAZ-1 study receiving IMFINZI (n=338), discontinuation due to
adverse reactions occurred in 6% of the patients receiving IMFINZI
plus chemotherapy. Serious adverse reactions occurred in 47% of
patients receiving IMFINZI plus chemotherapy. The most frequent
serious adverse reactions reported in at least 2% of patients were
cholangitis (7%), pyrexia (3.8%), anemia (3.6%), sepsis (3.3%) and
acute kidney injury (2.4%). Fatal adverse reactions occurred in
3.6% of patients receiving IMFINZI plus chemotherapy. These include
ischemic or hemorrhagic stroke (4 patients), sepsis (2 patients),
and upper gastrointestinal hemorrhage (2 patients).
- In patients with unresectable HCC in the HIMALAYA study
receiving IMFINZI and IMJUDO (n=388), the most common adverse
reactions (occurring in ≥20% of patients) were rash (32%), diarrhea
(27%), fatigue (26%), pruritus (23%), musculoskeletal pain (22%),
and abdominal pain (20%).
- In patients with unresectable HCC in the HIMALAYA study
receiving IMFINZI and IMJUDO (n=388), serious adverse reactions
occurred in 41% of patients. Serious adverse reactions in >1% of
patients included hemorrhage (6%), diarrhea (4%), sepsis (2.1%),
pneumonia (2.1%), rash (1.5%), vomiting (1.3%), acute kidney injury
(1.3%), and anemia (1.3%). Fatal adverse reactions occurred in 8%
of patients who received IMFINZI and IMJUDO, including death (1%),
hemorrhage intracranial (0.5%), cardiac arrest (0.5%), pneumonitis
(0.5%), hepatic failure (0.5%), and immune-mediated hepatitis
(0.5%). Permanent discontinuation of treatment regimen due to an
adverse reaction occurred in 14% of patients.
- In patients with advanced or recurrent dMMR endometrial cancer
in the DUO-E study receiving IMFINZI in combination with
carboplatin and paclitaxel followed by IMFINZI as a single-agent
(n=44), the most common adverse reactions, including laboratory
abnormalities (occurring in >20% of patients) were peripheral
neuropathy (61%), musculoskeletal pain (59%), nausea (59%),
alopecia (52%), fatigue (41%), abdominal pain (39%), constipation
(39%), rash (39%), decreased magnesium (36%), increased ALT (32%),
increased AST (30%), diarrhea (27%), vomiting (27%), cough (27%),
decreased potassium (25%), dyspnea (25%), headache (23%), increased
alkaline phosphatase (20%), and decreased appetite (18%). The most
common Grade 3 or 4 adverse reactions (≥3%) were constipation
(4.5%) and fatigue (4.5%).
- In patients with advanced or recurrent dMMR endometrial cancer
in the DUO-E study receiving IMFINZI in combination with
carboplatin and paclitaxel followed by IMFINZI as a single-agent
(n=44), permanent discontinuation of IMFINZI due to adverse
reactions occurred in 11% of patients. Serious adverse reactions
occurred in 30% of patients who received IMFINZI with carboplatin
and paclitaxel; the most common serious adverse reactions (≥4%)
were constipation (4.5%) and rash (4.5%).
The safety and effectiveness of IMFINZI and IMJUDO have not been
established in pediatric patients.
Indications:
IMFINZI is indicated for the treatment of adult patients with
unresectable Stage III non-small cell lung cancer (NSCLC) whose
disease has not progressed following concurrent platinum-based
chemotherapy and radiation therapy.
IMFINZI, in combination with IMJUDO and platinum-based
chemotherapy, is indicated for the treatment of adult patients with
metastatic NSCLC with no sensitizing epidermal growth factor
receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK)
genomic tumor aberrations.
IMFINZI, in combination with etoposide and either carboplatin or
cisplatin, is indicated for the first-line treatment of adult
patients with extensive-stage small cell lung cancer (ES-SCLC).
IMFINZI, in combination with gemcitabine and cisplatin, is
indicated for the treatment of adult patients with locally advanced
or metastatic biliary tract cancer (BTC).
IMFINZI in combination with IMJUDO is indicated for the
treatment of adult patients with unresectable hepatocellular
carcinoma (uHCC).
IMFINZI in combination with carboplatin and paclitaxel followed
by IMFINZI as a single agent is indicated for the treatment of
adult patients with primary advanced or recurrent endometrial
cancer that is mismatch repair deficient (dMMR).
Please see additional Important Safety Information throughout
and Full Prescribing Information including Medication Guide for
IMFINZI and IMJUDO.
You may report side effects related to AstraZeneca products
(opens new window).
Notes
Muscle-invasive bladder cancer
Bladder cancer is the 9th most common cancer in the world, with
more than 614,000 patients diagnosed each year.5 The most common
type of bladder cancer is urothelial carcinoma, which begins in the
urothelial cells of the urinary tract.6
Muscle-invasive bladder cancer, named for its growth into the
muscle wall of the bladder, accounts for about a quarter of all
bladder cancer cases.1,2 Approximately 50% of patients who undergo
bladder removal surgery experience disease recurrence.4 Treatment
options that prevent disease recurrence after surgery are
critically needed.
NIAGARA
NIAGARA is a randomized, open-label, multi-center, global Phase
III trial evaluating IMFINZI as treatment for patients with MIBC
before and after radical cystectomy. In the trial, 1063 patients
were randomised to receive IMFINZI plus chemotherapy or
chemotherapy alone prior to cystectomy, followed by IMFINZI or no
further treatment after surgery.
The trial is being conducted at 192 centers across 22 countries
and regions including in North America, South America, Europe,
Australia and Asia. Its dual primary endpoints are EFS, defined as
the time from treatment randomization to an event like tumor
recurrence or progression and pathologic complete response. Key
secondary endpoints are OS and safety.
IMFINZI
IMFINZI® (durvalumab) is a human monoclonal antibody that binds
to the PD-L1 protein and blocks the interaction of PD-L1 with the
PD-1 and CD80 proteins, countering the tumor's immune-evading
tactics and releasing the inhibition of immune responses.
IMFINZI is the only approved immunotherapy and the global
standard of care in the curative-intent setting of unresectable,
Stage III non-small cell lung cancer (NSCLC) in patients whose
disease has not progressed after chemoradiation therapy. IMFINZI is
also approved for the treatment of extensive-stage small cell lung
cancer (SCLC) and in combination with a short course of IMJUDO®
(tremelimumab) and chemotherapy for the treatment of metastatic
NSCLC.
IMFINZI in combination with neoadjuvant platinum-containing
chemotherapy before surgery and as adjuvant monotherapy after
surgery has been approved in Switzerland for the treatment of adult
patients with resectable NSCLC and no known epidermal growth factor
receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK)
rearrangements.
In addition to its indications in lung cancers, IMFINZI is
approved in combination with chemotherapy (gemcitabine plus
cisplatin) in locally advanced or metastatic biliary tract cancer
and in combination with IMJUDO in unresectable hepatocellular
carcinoma (HCC). IMFINZI is also approved as a monotherapy in
unresectable HCC in Japan and the EU and in combination with
chemotherapy (carboplatin plus paclitaxel) followed by IMFINZI
monotherapy in primary advanced or recurrent endometrial cancer
that is mismatch repair deficient in the US.
Since the first approval in May 2017, more than 220,000 patients
have been treated with IMFINZI. As part of a broad development
program, IMFINZI is being tested as a single treatment and in
combinations with other anti-cancer treatments for patients with
SCLC, NSCLC, breast cancer, several gastrointestinal and
gynecologic cancers, and other solid tumors.
IMFINZI is being tested across early- and late-stage bladder
cancer in various treatment combinations, including in non-muscle
invasive disease (POTOMAC), patients with MIBC who are
cisplatin-ineligible or refusing cisplatin (VOLGA) and locally
advanced or metastatic disease (NILE).
AstraZeneca in immuno-oncology (IO)
AstraZeneca is a pioneer in introducing the concept of
immunotherapy into dedicated clinical areas of high unmet medical
need. The Company has a comprehensive and diverse IO portfolio and
pipeline anchored in immunotherapies designed to overcome evasion
of the anti-tumor immune response and stimulate the body’s immune
system to attack tumors.
AstraZeneca strives to redefine cancer care and help transform
outcomes for patients with IMFINZI as a monotherapy and in
combination with IMJUDO as well as other novel immunotherapies and
modalities. The Company is also investigating next-generation
immunotherapies like bispecific antibodies as well as therapeutics
that harness different aspects of immunity to target cancer,
including cell therapy and T cell engagers.
AstraZeneca is pursuing an innovative clinical strategy to bring
IO-based therapies that deliver long-term survival to new settings
across a wide range of cancer types. The Company is focused on
exploring novel combination approaches to help prevent treatment
resistance and drive longer immune responses. With an extensive
clinical program, the Company also champions the use of IO
treatment in earlier disease stages, where there is the greatest
potential for cure.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the
ambition to provide cures for cancer in every form, following the
science to understand cancer and all its complexities to discover,
develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers.
It is through persistent innovation that AstraZeneca has built one
of the most diverse portfolios and pipelines in the industry, with
the potential to catalyze changes in the practice of medicine and
transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day,
eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca is a global, science-led biopharmaceutical company
that focuses on the discovery, development and commercialization of
prescription medicines in Oncology, Rare Diseases and
BioPharmaceuticals, including Cardiovascular, Renal &
Metabolism, and Respiratory & Immunology. Based in Cambridge,
UK, AstraZeneca operates in over 125 countries, and its innovative
medicines are used by millions of patients worldwide. For more
information, please visit www.astrazeneca-us.com and follow us on
social media @AstraZeneca.
References
1.
Burger M, et al. Epidemiology and Risk
Factors of Urothelial Bladder Cancer. Eur Urol.
2013;63(2):234-241.
2.
National Collaborating Centre for Cancer.
Bladder Cancer: Diagnosis and Management. London: National
Institute for Health and Care Excellence (NICE). Available at:
https://www.ncbi.nlm.nih.gov/books/NBK356289/. Accessed June
2024.
3.
Cerner CancerMPact database. Accessed June
2024. Reflects epidemiology estimates across G8 countries (US, EU,
Japan, China).
4.
Witjes JA, et al. EAU Guidelines on
muscle-invasive and metastatic bladder cancer. Eur Urol.
2021;1-94.
5.
World Health Organization. International
Agency for Research on Cancer. Bladder Fact Sheet. Available at:
https://gco.iarc.who.int/media/globocan/factsheets/cancers/30-bladder-fact-sheet.pdf.
Accessed June 2024.
6.
American Cancer Society. What Is Bladder
Cancer? Available at:
https://www.cancer.org/cancer/bladder-cancer/about/what-is-bladder-cancer.html.
Accessed June 2024.
US-91093 Last Updated 6/24
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240625461835/en/
Media Inquiries Brendan McEvoy +1 302 885 2677 Chelsea
Tressler +1 302 885 2677 US Media Mailbox:
usmediateam@astrazeneca.com
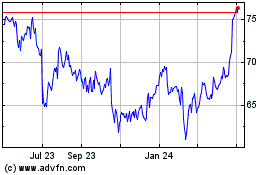
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Oct 2024 to Nov 2024
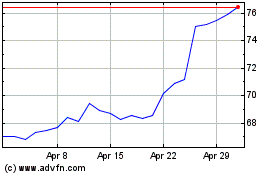
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Nov 2023 to Nov 2024