FALSE000133349300013334932024-11-062024-11-06
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, D.C. 20549
FORM 8-K
CURRENT REPORT
PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
Date of Report (date of earliest event reported): November 6, 2024
EHEALTH, INC.
(Exact Name of Registrant as Specified in its Charter) | | | | | | | | |
| | |
| Delaware | 001-33071 | 56-2357876 |
| (State or other jurisdiction of incorporation) | (Commission File Number) | (I.R.S. Employer Identification No.) |
13620 RANCH ROAD 620 N, SUITE A250
AUSTIN, TX 78717
(Address of principal executive offices) (Zip Code)
(737) 248-2340
(Registrant’s telephone number, including area code)
Not applicable
(Former name or former address, if changed since last report.)
Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions:
☐ Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425)
☐ Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12)
☐ Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b))
☐ Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c))
Securities registered pursuant to Section 12(b) of the Act: | | | | | | | | | | | | | | |
| Title of each class | | Trading Symbol(s) | | Name of each exchange on which registered |
| Common Stock, par value $0.001 per share | | EHTH | | The Nasdaq Stock Market LLC |
Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (17 CFR §230.405) or Rule 12b-2 of the Securities Exchange Act of 1934 (17 CFR §240.12b-2). Emerging growth company ☐
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ¨
| | | | | | | | |
| Item 2.02 | | Results of Operations and Financial Condition. |
On November 6, 2024, eHealth, Inc. (the “Company”) issued a press release announcing its financial results for the three and nine months ended September 30, 2024 and its financial condition as of September 30, 2024. A copy of the press release is furnished as Exhibit 99.1 to this Current Report on Form 8-K and is incorporated herein by reference.
On November 6, 2024, the Company posted supplemental investor material on its investor relations webpage at https://ir.ehealthinsurance.com. The Company intends to use its investor relations webpage as a means of disclosing material non-public information and for complying with its disclosure obligations under Regulation FD. A copy of the supplemental investor materials is also furnished as Exhibit 99.2 to this Current Report on Form 8-K and is incorporated herein by reference.
| | | | | | | | |
| Item 9.01 | | Financial Statements and Exhibits. |
(d) Exhibits
| | | | | |
| Exhibit No. | Description |
| 99.1 | |
| 99.2 | |
| 104 | Cover Page Interactive Data File (embedded within the Inline XBRL document) |
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned hereunto duly authorized.
| | | | | | | | |
| | |
| | eHealth, Inc. |
| Date: | November 6, 2024 | /s/ John Dolan |
| | John Dolan Chief Financial Officer (Principal Financial Officer) |
eHealth, Inc. Announces Third Quarter 2024 Results
Third quarter performance driven by strong Medicare segment execution YoY
Entered AEP on solid financial and operational foundation
Completed extension of term loan at improved interest rate terms
AUSTIN, Texas — November 6, 2024 — eHealth, Inc. (Nasdaq: EHTH), a leading private online health insurance marketplace, today announced its financial results for the third quarter ended September 30, 2024.
| | | | | | | | |
| CEO Comments | | |
| | |
“In the third quarter, eHealth achieved our revenue and profitability targets, delivered significant growth in Medicare application volume, and completed our final preparations for the Annual Enrollment Period (“AEP”). We maintained this strong momentum in the first weeks of the AEP, with call volume, online visits to our platform and conversion rates across enrollment channels, up meaningfully year-over-year and exceeding our expectations. We have also implemented a multi-faceted plan to serve eHealth's existing members, including dedicated advisor support and plan monitor tools available on our online platform, to ensure customers continue to be enrolled in coverage that best fits their needs.” – Fran Soistman, Chief Executive Officer |
■Q3 2024 Medicare submissions(a) across our core agency and carrier-dedicated Amplify platforms grew 22% compared to Q3 2023, driven primarily by Medicare Advantage (“MA”) submissions growth of 26% year-over-year.
■Q3 2024 total Medicare approved members increased 6% year-over-year, driven mostly by a 14% increase in Q3 2024 MA approved members year-over-year.
■Q3 2024 total revenue of $58.4 million decreased 10% year-over-year, driven primarily by lower positive net adjustment revenue, as compared to Q3 2023 total revenue of $64.7 million.
■Q3 2024 positive net adjustment revenue of $1.2 million compared to $12.2 million in Q3 2023.
■Q3 2024 Non-GAAP total revenue excluding net adjustment revenue(1) increased 9% year-over-year.
■Q3 2024 total acquisition cost per MA-equivalent approved member declined 16% compared to Q3 2023.
■Q3 2024 GAAP net loss of $42.5 million increased 15%, compared to Q3 2023 GAAP net loss of $37.0 million.
■Q3 2024 Non-GAAP net loss(1) of $43.3 million, which excludes the post-tax impact of positive net adjustment revenue and restructuring charges, improved 6% year-over-year.
■Q3 2024 adjusted EBITDA(1) of $(34.8) million compared to Q3 2023 adjusted EBITDA(1) of $(28.1) million; Q3 2024 adjusted EBITDA excluding net adjustment revenue(1) improved $4.3 million year-over-year, driven primarily by MA approved member growth, improved Medicare acquisition costs and continued fixed cost reduction efforts.
■Successfully completed our AEP preparations; achieved our licensed agent headcount targets and conducted a robust training program, developed our integrated brand marketing strategy and made further enhancements to our online platform.
■Amended term loan credit agreement to extend maturity date to February 2026 with improved interest rate terms.
■Cash, cash equivalents and marketable securities of $117.8 million as of September 30, 2024.
■Commissions receivable balance of $814.0 million as of September 30, 2024.
__________
Note: See the tables at the end of this press release for a reconciliation of our GAAP financial measures to our non-GAAP financial measures for the relevant periods and footnote (1) on page 15 at the end of this press release for definitions of our non-GAAP financial measures. (a) Submissions describe applications that are submitted by individuals online through our eHealth platform or completed with the assistance of our benefit advisors where the individual provides authorization to the benefit advisor to submit the application to the insurance carrier partner. The individual may have additional actions to take before the application will be reviewed by the insurance carrier and not all submissions ultimately become approved members.
2024 Guidance
Based on information available as of November 6, 2024, we are reiterating our guidance for the full year ending December 31, 2024. These expectations are forward-looking statements and we assume no obligation to update these statements. Actual results may be materially different and are affected by the risk factors and uncertainties identified in this press release and in eHealth’s annual and quarterly reports filed with the Securities and Exchange Commission.
The following guidance is for the full year ending December 31, 2024:
•Total revenue is expected to be in the range of $470.0 million to $495.0 million.
•GAAP net income (loss) is expected to be in the range of $(36.5) million to $(22.0) million.
•Adjusted EBITDA(1) is expected to be in the range of $7.5 million to $25.0 million.
•Operating cash flow is expected to be in the range of $(10.0) million to $0.0 million.
The above guidance includes the expected impact of positive net adjustment revenue in the range of $14 to $20 million. Excluding the impact of positive net adjustment revenue in both years, the mid-point of our 2024 guidance reflects approximately 15% growth in Non-GAAP total revenue excluding net adjustment revenue(1) and a substantial improvement in Non-GAAP net income (loss)(1) and adjusted EBITDA excluding net adjustment revenue(1) year-over-year.
__________
Note: See accompanying footnotes on page 15.
Webcast and Conference Call Information
A webcast and conference call will be held today, Wednesday, November 6, 2024 at 8:30 a.m. Eastern Time / 7:30 a.m. Central Time. Individuals interested in listening to the conference call may do so by dialing (800) 343-5172. The participant passcode is 1401106. The live and archived webcast of the call will also be available under “Events & Presentations” on the Investor Relations page of our website at https://ir.ehealthinsurance.com.
About eHealth, Inc.
We’re Matchmakers. For over 25 years, eHealth has helped millions of Americans find the healthcare coverage that fits their needs at a price they can afford. As a leading independent licensed insurance agency and advisor, eHealth offers access to over 180 health insurers, including national and regional companies.
For more information, visit eHealth.com or follow us on LinkedIn, Facebook, Instagram, and X. Open positions can be found on our career page.
Forward-Looking Statements
This press release contains statements that are forward-looking statements as defined within the Private Securities Litigation Reform Act of 1995. These include statements regarding our expectations regarding our business, operations and strategy; our estimates regarding total membership, Medicare, individual and family plan, ancillary products and small business memberships; our estimates regarding constrained lifetime values of commissions per approved member by product category; our estimates regarding costs per approved member; our 2024 annual guidance for total revenue, GAAP net income (loss), adjusted EBITDA and operating cash flow; our estimates for positive net adjustment revenue and its expected impact on our 2024 annual guidance; the impact of our efforts to prepare for the annual enrollment period, and other statements regarding our future operations, financial condition, prospects and business strategies.
These forward-looking statements are inherently subject to various risks and uncertainties that could cause actual results to differ materially from the statements made. In particular, we are required by Accounting Standards Codification 606 — Revenue from Contracts with Customers to make numerous assumptions that are based on historical trends and our
management’s judgment. These assumptions may change over time and have a material impact on our revenue recognition, guidance, and results of operations. Please review the assumptions stated in this press release carefully.
The risks and uncertainties that could cause our results to differ materially from those expressed or implied by such forward-looking statements include, but are not limited to, our ability to retain existing members and enroll new members during the annual healthcare open enrollment period, the Medicare annual enrollment period, the Medicare Advantage annual open enrollment period and other special enrollment periods; changes in laws, regulations and guidelines, including in connection with healthcare reform or with respect to the marketing and sale of Medicare plans, such as the Policy and Technical Changes to Medicare Advantage for Contract Year 2025 released by CMS on April 4, 2024; competition, including competition from government-run health insurance exchanges and other sources; the seasonality of our business and the fluctuation of our operating results; our ability to accurately estimate membership, lifetime value of commissions and commissions receivable; changes in product offerings among carriers on our ecommerce platform and changes in our estimated conversion rate of an approved member to a paying member and the resulting impact of each on our commission revenue; the concentration of our revenue with a small number of health insurance carriers; our ability to execute on our growth strategy and other business initiatives; changes in our management or other key employees; our ability to hire, train, retain and ensure the productivity of licensed insurance agents, or benefit advisors, and other personnel; exposure to security risks and our ability to safeguard the security and privacy of confidential data; our relationships with health insurance carriers; the success of our carrier advertising and sponsorship program; our success in marketing and selling health insurance plans and our unit cost of acquisition; our ability to effectively manage our operations as our business evolves and execute on our business plan and other strategic initiatives; the need for health insurance carrier and regulatory approvals in connection with the marketing of Medicare-related insurance products; changes in the market for private health insurance; consumer satisfaction of our service and actions we take to improve the quality of enrollments; changes in member conversion rates; changes in commission rates; our ability to sell qualified health insurance plans to subsidy-eligible individuals and to enroll subsidy-eligible individuals through government-run health insurance exchanges; our ability to derive desired benefits from investments in our business, including membership growth and retention initiatives; our reliance on marketing partners; the success and cost of our marketing efforts, including branding, online advertising, direct-to-consumer mail, email, social media, telephone, television, radio and other marketing efforts; timing of receipt and accuracy of commission reports; payment practices of health insurance carriers; dependence on our operations in China; the restrictions in our debt obligations; the restrictions in our investment agreement with our convertible preferred stock investor; our ability to raise additional capital; compliance with insurance, privacy, cybersecurity and other laws and regulations; the outcome of litigation in which we may from time to time be involved; the performance, reliability and availability of our information technology systems, ecommerce platform and underlying network infrastructure, including any new systems we may implement; public health crises, pandemics, natural disasters, changing climate conditions and other extreme events; general economic conditions, including inflation, recession, financial, banking and credit market disruptions; and our ability to effectively administer our self-insurance program. Other factors that could cause operating, financial and other results to differ are described in our most recent Quarterly Report on Form 10-Q or Annual Report on Form 10-K filed with the Securities and Exchange Commission and available on the Investor Relations page of our website at https://ir.ehealthinsurance.com and on the Securities and Exchange Commission’s website at www.sec.gov.
All forward-looking statements in this press release are based on information available to us as of the date hereof, and we do not assume any obligation to update the forward-looking statements provided to reflect events that occur or circumstances that exist after the date on which they were made, except as required by law.
Investor Relations Contact
Kate Sidorovich, CFA
Senior Vice President, Investor Relations & Strategy
investors@ehealth.com
https://ir.ehealthinsurance.com
EHEALTH, INC.
CONDENSED CONSOLIDATED BALANCE SHEETS
(in thousands, unaudited)
| | | | | | | | | | | |
| September 30, 2024 | | December 31, 2023 |
| Assets | | | |
| Current assets: | | | |
| Cash and cash equivalents | $ | 64,032 | | | $ | 115,722 | |
| Short-term marketable securities | 53,750 | | | 5,930 | |
| Accounts receivable | 5,864 | | | 3,993 | |
| Contract assets – commissions receivable – current | 197,591 | | | 244,663 | |
| Prepaid expenses and other current assets | 19,630 | | | 12,044 | |
| Total current assets | 340,867 | | | 382,352 | |
| Contract assets – commissions receivable – non-current | 616,445 | | | 673,514 | |
| Property and equipment, net | 4,770 | | | 4,864 | |
| | | |
| Operating lease right-of-use assets | 12,442 | | | 22,767 | |
| Restricted cash | 3,090 | | | 3,090 | |
| Other assets | 24,377 | | | 26,758 | |
| | | |
| | | |
| Total assets | $ | 1,001,991 | | | $ | 1,113,345 | |
| | | |
| Liabilities, convertible preferred stock and stockholders’ equity | | | |
| Current liabilities: | | | |
| Accounts payable | $ | 5,407 | | | $ | 7,197 | |
| Accrued compensation and benefits | 26,207 | | | 40,800 | |
| Accrued marketing expenses | 9,208 | | | 20,340 | |
| | | |
| | | |
| Lease liabilities – current | 7,429 | | | 7,070 | |
| | | |
| Other current liabilities | 5,597 | | | 3,131 | |
| Total current liabilities | 53,848 | | | 78,538 | |
| Long-term debt | 69,155 | | | 67,754 | |
| | | |
| Deferred income taxes – non-current | 25,347 | | | 29,687 | |
| Lease liabilities – non-current | 22,349 | | | 28,333 | |
| Other non-current liabilities | 4,821 | | | 4,949 | |
| Total liabilities | 175,520 | | | 209,261 | |
| Convertible preferred stock | 327,125 | | | 298,053 | |
| Stockholders’ equity: | | | |
| | | |
| Common stock | 43 | | | 41 | |
| Additional paid-in capital | 812,538 | | | 798,786 | |
| Treasury stock, at cost | (199,998) | | | (199,998) | |
| Retained earnings (accumulated deficit) | (113,363) | | | 7,284 | |
| Accumulated other comprehensive income (loss) | 126 | | | (82) | |
| Total stockholders’ equity | 499,346 | | | 606,031 | |
| Total liabilities, convertible preferred stock and stockholders’ equity | $ | 1,001,991 | | | $ | 1,113,345 | |
EHEALTH, INC.
CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS
(in thousands, except per share amounts, unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | | | Nine Months Ended
September 30, | | |
| 2024 | | 2023 | | % Change | | 2024 | | 2023 | | % Change |
| Revenue: | | | | | | | | | | | |
| Commission | $ | 48,222 | | $ | 57,239 | | (16) | % | | $ | 185,996 | | $ | 185,428 | | — | % |
| Other | 10,187 | | 7,479 | | 36 | % | | 31,233 | | 19,781 | | 58 | % |
| Total revenue | 58,409 | | 64,718 | | (10) | % | | 217,229 | | 205,209 | | 6 | % |
Operating costs and expenses(a): | | | | | | | | | | | |
| | | | | | | | | | | |
Marketing and advertising(8) | 29,665 | | 29,035 | | 2 | % | | 95,185 | | 85,343 | | 12 | % |
Customer care and enrollment(8) | 39,321 | | 38,901 | | 1 | % | | 100,773 | | 93,951 | | 7 | % |
Technology and content(8) | 12,264 | | 13,241 | | (7) | % | | 38,613 | | 42,047 | | (8) | % |
General and administrative(8) | 20,297 | | 22,937 | | (12) | % | | 62,318 | | 72,310 | | (14) | % |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment, restructuring and other charges | 61 | | — | | * | | 9,409 | | — | | * |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Total operating costs and expenses | 101,608 | | 104,114 | | (2) | % | | 306,298 | | 293,651 | | 4 | % |
| Loss from operations | (43,199) | | (39,396) | | (10) | % | | (89,069) | | (88,442) | | (1) | % |
| Interest expense | (2,859) | | (2,822) | | (1) | % | | (8,517) | | (8,122) | | (5) | % |
| Other income, net | 1,699 | | 2,684 | | (37) | % | | 6,425 | | 7,500 | | (14) | % |
| Loss before income taxes | (44,359) | | (39,534) | | (12) | % | | (91,161) | | (89,064) | | (2) | % |
| Benefit from income taxes | (1,886) | | (2,509) | | | | (3,736) | | (8,660) | | |
| Net loss | (42,473) | | (37,025) | | (15) | % | | (87,425) | | (80,404) | | (9) | % |
| Preferred stock dividends | (5,643) | | (5,320) | | | | (16,603) | | (15,644) | | |
| Change in preferred stock redemption value | (5,832) | | (4,898) | | | | (16,619) | | (12,158) | | |
| | | | | | | | | | | |
| Net loss attributable to common stockholders | $ | (53,948) | | $ | (47,243) | | (14) | % | | $ | (120,647) | | $ | (108,206) | | (11) | % |
| | | | | | | | | | | |
Net loss per share attributable to common stockholders: | | | | | | | | | | | |
Basic and diluted | $ | (1.83) | | $ | (1.68) | | (9) | % | | $ | (4.13) | | $ | (3.88) | | (6) | % |
| | | | | | | | | | | |
| Weighted-average number of shares used in per share: | | | | | | | | | | | |
Basic and diluted | 29,485 | | 28,114 | | 5 | % | | 29,211 | | 27,863 | | 5 | % |
| | | | | | | | | | | |
_____________________________ (a) Includes stock-based compensation expense as follows: |
| Marketing and advertising | $ | 437 | | $ | 605 | | | | $ | 1,792 | | $ | 1,598 | | |
| Customer care and enrollment | 452 | | 836 | | | | 1,487 | | 2,229 | | |
| Technology and content | 845 | | 1,306 | | | | 2,598 | | 3,384 | | |
| General and administrative | 2,745 | | 3,807 | | | | 9,248 | | 10,530 | | |
| | | | | | | | | | | |
| Total stock-based compensation expense | $ | 4,479 | | $ | 6,554 | | (32) | % | | $ | 15,125 | | $ | 17,741 | | (15) | % |
| | | | | | | | | | | |
Non-GAAP Results(1): | | | | | | | | | | | |
Adjusted EBITDA(1) | $ | (34,832) | | $ | (28,097) | | (24) | % | | $ | (52,024) | | $ | (55,560) | | 6 | % |
Adjusted EBITDA margin(1) | (60) | % | | (43) | % | | | | (24) | % | | (27) | % | | |
__________
* Percentage calculated is not meaningful.
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
CONDENSED CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands, unaudited)
| | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | Nine Months Ended
September 30, | | |
| | 2024 | | 2023 | | 2024 | | 2023 | | | | |
| Operating activities: | | | | | | | | | | | |
| Net loss | $ | (42,473) | | | $ | (37,025) | | | $ | (87,425) | | | $ | (80,404) | | | | | |
| Adjustments to reconcile net loss to net cash provided by (used in) operating activities: | | | | | | | | | | | |
| Depreciation and amortization | 473 | | | 614 | | | 1,481 | | | 1,908 | | | | | |
| Amortization of internally developed software | 3,354 | | | 4,131 | | | 11,030 | | | 13,233 | | | | | |
| | | | | | | | | | | |
| Stock-based compensation expense | 4,479 | | | 6,554 | | | 15,125 | | | 17,741 | | | | | |
| Deferred income taxes | (1,709) | | | (2,611) | | | (4,340) | | | (9,311) | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment charges | — | | | — | | | 7,413 | | | — | | | | | |
| Other non-cash items | 74 | | | 106 | | | (43) | | | 5 | | | | | |
| Changes in operating assets and liabilities: | | | | | | | | | | | |
| Accounts receivable | (4,681) | | | 121 | | | (1,871) | | | 2,110 | | | | | |
| Contract assets – commissions receivable | 17,885 | | | 9,148 | | | 104,582 | | | 104,160 | | | | | |
| Prepaid expenses and other assets | (11,327) | | | (12,473) | | | (9,896) | | | (12,597) | | | | | |
| Accounts payable | 509 | | | 802 | | | (1,965) | | | 181 | | | | | |
| Accrued compensation and benefits | 6,195 | | | 5,823 | | | (14,593) | | | 6,102 | | | | | |
| Accrued marketing expenses | 1,366 | | | 989 | | | (11,132) | | | (16,347) | | | | | |
| Deferred revenue | (1,173) | | | 1,040 | | | 861 | | | 1,323 | | | | | |
| | | | | | | | | | | |
| Accrued expenses and other liabilities | (2,255) | | | (1,900) | | | 69 | | | (1,410) | | | | | |
| Net cash provided by (used in) operating activities | (29,283) | | | (24,681) | | | 9,296 | | | 26,694 | | | | | |
| Investing activities: | | | | | | | | | | | |
| Capitalized internal-use software and website development costs | (3,191) | | | (2,826) | | | (8,070) | | | (7,028) | | | | | |
| Purchases of property and equipment and other assets | (998) | | | (1,386) | | | (1,463) | | | (1,759) | | | | | |
| Purchases of marketable securities | (48,489) | | | — | | | (85,880) | | | (48,602) | | | | | |
| Proceeds from redemption and maturities of marketable securities | 20,000 | | | 28,500 | | | 39,000 | | | 40,900 | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Net cash provided by (used in) investing activities | (32,678) | | | 24,288 | | | (56,413) | | | (16,489) | | | | | |
| Financing activities: | | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Net proceeds from exercise of common stock options and employee stock purchases | — | | | — | | | 354 | | | 262 | | | | | |
| Repurchase of shares to satisfy employee tax withholding obligations | (450) | | | (884) | | | (2,301) | | | (1,935) | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Principal payments in connection with leases | — | | | (8) | | | (4) | | | (33) | | | | | |
| Payments of preferred stock dividends | — | | | — | | | (2,740) | | | (873) | | | | | |
Net cash used in financing activities | (450) | | | (892) | | | (4,691) | | | (2,579) | | | | | |
| Effect of exchange rate changes on cash, cash equivalents and restricted cash | 99 | | | 69 | | | 118 | | | (58) | | | | | |
Net increase (decrease) in cash, cash equivalents and restricted cash | (62,312) | | | (1,216) | | | (51,690) | | | 7,568 | | | | | |
| Cash, cash equivalents and restricted cash at beginning of period | 129,434 | | | 156,424 | | | 118,812 | | | 147,640 | | | | | |
| Cash, cash equivalents and restricted cash at end of period | $ | 67,122 | | | $ | 155,208 | | | $ | 67,122 | | | $ | 155,208 | | | | | |
EHEALTH, INC.
SEGMENT INFORMATION
(in thousands, unaudited)
We evaluate our business performance and manage our operations as two distinct reporting segments: Medicare and Employer and Individual (“E&I”). In the fourth quarter of 2023, the Individual, Family and Small Business segment was renamed “Employer and Individual”. The E&I segment name change was to the name only and had no impact on our historical financial position, results of operations, cash flow or segment level results previously reported. This identification of reportable segments is consistent with how the segments report to and are managed by our chief executive officer, who is our chief operating decision maker (“CODM”). The Medicare segment consists primarily of amounts earned from our sale of Medicare-related health insurance plans, including Medicare Advantage, Medicare Supplement and Medicare Part D prescription drug plans (collectively, the “Medicare Plans”), fees earned for the performance of administrative services, amounts earned from our non-broker of record arrangements, our performance of various post-enrollment services for members and to a lesser extent, amounts earned from our sale of ancillary products sold to our Medicare-eligible customers, including but not limited to, dental and vision plans, as well as amounts we are paid in connection with our advertising program for marketing and other services. The E&I segment consists primarily of amounts earned from our sale of individual, family and small business health insurance plans, including both qualified and non-qualified plans, and ancillary products sold to our non-Medicare-eligible customers, including but not limited to, dental, vision, and short-term insurance. To a lesser extent, the E&I segment consists of amounts earned from our online sponsorship and advertising program that allows carriers to purchase advertising space in specific markets in a sponsorship area on our website and our technology licensing and lead referral activities.
Marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses that are directly attributable to a segment are reported within the applicable segment. Indirect marketing and advertising, customer care and enrollment and technology and content operating expenses are allocated to each segment based on usage. Corporate consists of other general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, which are managed in a corporate shared services environment and, since they are not the responsibility of segment operating management, are not allocated to the reportable segments and are instead reported within Corporate. Our results below reflect our updated methodology used in allocating certain expenses beginning in the first quarter of fiscal 2024, and results from the prior period presented have been recast to conform with the current period presentation. See accompanying footnotes on page 15 for further information.
The performance of each reportable segment is evaluated based on several factors, including revenue and segment profit (loss), which is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, interest expense and other income (expense), net. Senior management uses segment profit (loss) to evaluate segment performance because they believe this measure is indicative of performance trends and the overall earnings potential of each segment.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | % Change | | Nine Months Ended
September 30, | | % Change |
| | 2024 | | 2023 | | | 2024 | | 2023 | |
| Revenue: | | | | | | | | | | | |
| Medicare | $ | 53,221 | | | $ | 55,523 | | | (4) | % | | $ | 194,857 | | | $ | 172,787 | | | 13 | % |
Employer and Individual | 5,188 | | | 9,195 | | | (44) | % | | 22,372 | | | 32,422 | | | (31) | % |
| Total revenue | $ | 58,409 | | | $ | 64,718 | | | (10) | % | | $ | 217,229 | | | $ | 205,209 | | | 6 | % |
| | | | | | | | | | | |
Segment profit (loss)(8): | | | | | | | | | | | |
| Medicare | $ | (17,933) | | | $ | (15,331) | | | (17) | % | | $ | (8,350) | | | $ | (17,979) | | | 54 | % |
Employer and Individual | (799) | | | 4,810 | | | (117) | % | | 4,743 | | | 19,372 | | | (76) | % |
Segment profit (loss) | (18,732) | | | (10,521) | | | (78) | % | | (3,607) | | | 1,393 | | | (359) | % |
Corporate(8) | (16,100) | | | (17,576) | | | | | (48,417) | | | (56,953) | | | |
| Stock-based compensation expense | (4,479) | | | (6,554) | | | | | (15,125) | | | (17,741) | | | |
| | | | | | | | | | | |
| Depreciation and amortization | (3,827) | | | (4,745) | | | | | (12,511) | | | (15,141) | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Impairment, restructuring and other charges | (61) | | | — | | | | | (9,409) | | | — | | | |
| Interest expense | (2,859) | | | (2,822) | | | | | (8,517) | | | (8,122) | | | |
| Other income, net | 1,699 | | | 2,684 | | | | | 6,425 | | | 7,500 | | | |
Loss before income taxes | $ | (44,359) | | | $ | (39,534) | | | (12) | % | | $ | (91,161) | | | $ | (89,064) | | | (2) | % |
__________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
COMMISSION REVENUE
(in thousands, unaudited)
Our commission revenue results from approval of an application from health insurance carriers, which we define as our customers under Accounting Standards Codification 606 — Revenue from Contracts with Customers (“ASC 606”). Our commission revenue is primarily comprised of commissions from health insurance carriers which is computed using the estimated constrained lifetime values of commission payments that we expect to receive. Our commissions may include certain bonus payments, which are generally based on our attaining predetermined target sales levels or other objectives, as determined by the health insurance carriers. For Medicare Advantage and Medicare Part D prescription drug plans, our commissions also include regular payments related to administrative services we perform.
The following table presents commission revenue by product for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | % Change | | Nine Months Ended
September 30, | | % Change |
| 2024 | | 2023 | | | 2024 | | 2023 | |
| Medicare | | | | | | | | | | | |
| Medicare Advantage | $ | 39,463 | | | $ | 43,721 | | | (10) | % | | $ | 143,627 | | | $ | 143,231 | | | — | % |
| Medicare Supplement | 2,312 | | | 2,630 | | | (12) | % | | 11,835 | | | 7,786 | | | 52 | % |
| Medicare Part D | 843 | | | 2,046 | | | (59) | % | | 6,238 | | | 4,686 | | | 33 | % |
| Total Medicare | 42,618 | | | 48,397 | | | (12) | % | | 161,700 | | | 155,703 | | | 4 | % |
Individual and Family | | | | | | | | | | | |
| Non-Qualified Health Plans | (199) | | | 1,560 | | | (113) | % | | 1,834 | | | 6,904 | | | (73) | % |
| Qualified Health Plans | 602 | | | 681 | | | (12) | % | | 3,358 | | | 4,084 | | | (18) | % |
Total Individual and Family | 403 | | | 2,241 | | | (82) | % | | 5,192 | | | 10,988 | | | (53) | % |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| | | | | | | | | | | |
| Ancillary | 2,036 | | | 2,560 | | | (20) | % | | 7,279 | | | 7,503 | | | (3) | % |
| Small Business | 2,268 | | | 3,884 | | | (42) | % | | 8,447 | | | 12,557 | | | (33) | % |
| Commission Bonus and Other | 897 | | | 157 | | | 471 | % | | 3,378 | | | (1,323) | | | 355 | % |
| Total Commission Revenue | $ | 48,222 | | | $ | 57,239 | | | (16) | % | | $ | 185,996 | | | $ | 185,428 | | | — | % |
The following table presents a summary of commission revenue by segment for the periods indicated:
| | | | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | Nine Months Ended
September 30, | | |
| | 2024 | | 2023 | | 2024 | | 2023 | |
| Medicare | | | | | | | | | |
Commission revenue from members approved during the period | $ | 42,324 | | | $ | 39,169 | | | $ | 152,017 | | | $ | 131,792 | | | |
Net commission revenue from members approved in prior periods(a) | 1,090 | | | 9,291 | | | 12,773 | | | 22,746 | | | |
Total Medicare segment commission revenue | 43,414 | | | 48,460 | | | 164,790 | | | 154,538 | | | |
Employer and Individual | | | | | | | | | |
Commission revenue from members approved during the period | 2,848 | | | 3,829 | | | 11,790 | | | 13,835 | | | |
Commission revenue from renewals of small business members during the period | 1,852 | | | 2,028 | | | 7,022 | | | 7,299 | | | |
Net commission revenue from members approved in prior periods(a) | 108 | | | 2,922 | | | 2,394 | | | 9,756 | | | |
Total Employer and Individual segment commission revenue | 4,808 | | | 8,779 | | | 21,206 | | | 30,890 | | | |
Total commission revenue | $ | 48,222 | | | $ | 57,239 | | | $ | 185,996 | | | $ | 185,428 | | | |
_____________
(a) These amounts reflect our revised estimates of cash collections for certain members approved prior to the relevant reporting period that are recognized as adjustments to revenue within the relevant reporting period. The net commission revenue from members approved in prior periods, or net adjustment revenue, includes both increases in revenue for certain prior period cohorts as well as reductions in revenue for certain prior period cohorts. The total reductions to revenue from members approved in prior periods were $0.9 million and $0.8 million for the three months ended September 30, 2024 and 2023, respectively, and $4.5 million and $3.7 million for the nine months ended September 30, 2024 and 2023, respectively. These reductions to revenue primarily relate to the Medicare segment.
EHEALTH, INC.
SUMMARY OF SELECTED METRICS
(in thousands, except member and per member data, unaudited)
Selected Metrics — Third Quarter of 2024
| | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | % Change |
| 2024 | | 2023 | |
Approved Members(2)(a) | | | | | |
| Medicare | | | | | |
| Medicare Advantage | 40,141 | | 35,069 | | 14 | % |
| Medicare Supplement | 1,438 | | 3,010 | | (52) | % |
| Medicare Part D | 1,292 | | 2,480 | | (48) | % |
| Total Medicare | 42,871 | | 40,559 | | 6 | % |
| Individual and Family | 2,872 | | 3,727 | | (23) | % |
| Ancillary | 11,382 | | 12,877 | | (12) | % |
| Small Business | 1,141 | | 1,304 | | (13) | % |
| Total Approved Members | 58,266 | | 58,467 | | — | % |
(a) The shift of some carrier arrangements from broker of record to fee-based BPO during 2024 impacted the growth in approved members as only broker of record arrangements are reflected in approved members. |
| | | | | |
Constrained Lifetime Value of Commissions per Approved Member(3) | | | | | |
Medicare(b) | | | | | |
| Medicare Advantage | $ | 990 | | $ | 997 | | (1) | % |
| Medicare Supplement | 1,105 | | 833 | | 33 | % |
| Medicare Part D | 222 | | 235 | | (6) | % |
| Individual and Family | | | | | |
| Non-Qualified Health Plans | 314 | | 325 | | (3) | % |
| Qualified Health Plans | 311 | | 322 | | (3) | % |
| Ancillary | | | | | |
| Short-term | 144 | | 151 | | (5) | % |
| Dental | 118 | | 108 | | 9 | % |
| Vision | 78 | | 72 | | 8 | % |
| Small Business | 249 | | 226 | | 10 | % |
(b) Constraint for Medicare Advantage was 5.5% and 7% for the three months ended September 30, 2024 and 2023, respectively. Constraints for all other Medicare products remained the same for the periods presented. |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
Expense Metrics per Approved Member(4) | | | | | |
| Medicare | | | | | |
Customer care and enrollment cost per Medicare Advantage (“MA”)-equivalent approved member(8) | $ | 719 | | $ | 946 | | (24) | % |
| Variable marketing cost per MA-equivalent approved member | 537 | | 557 | | (4) | % |
| Total acquisition cost per MA-equivalent approved member | $ | 1,256 | | $ | 1,503 | | (16) | % |
Individual and Family Plan (“IFP”) | | | | | |
Customer care and enrollment cost per IFP-equivalent approved member(8) | $ | 359 | | $ | 256 | | 40 | % |
| Variable marketing cost per IFP-equivalent approved member | 118 | | 68 | | 74 | % |
| Total acquisition cost per IFP-equivalent approved member | $ | 477 | | $ | 324 | | 47 | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
__________Note: See accompanying footnotes on page 15.
EHEALTH, INC.
SUMMARY OF SELECTED METRICS
(in thousands, except member and per member data, unaudited)
Selected Metrics — Nine Months Ended September 30, 2024
| | | | | | | | | | | | | | | | | |
| Nine Months Ended
September 30, | | % Change |
| 2024 | | 2023 | |
Approved Members(2)(a) | | | | | |
| Medicare | | | | | |
| Medicare Advantage | 143,529 | | | 131,117 | | | 9 | % |
| Medicare Supplement | 9,574 | | | 10,518 | | | (9) | % |
| Medicare Part D | 6,335 | | | 9,274 | | | (32) | % |
| Total Medicare | 159,438 | | | 150,909 | | | 6 | % |
| Individual and Family | 13,540 | | | 18,111 | | | (25) | % |
| | | | | |
| | | | | |
| | | | | |
| Ancillary | 36,410 | | | 42,584 | | | (14) | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
| Small Business | 3,705 | | | 5,207 | | | (29) | % |
| Total Approved Members | 213,093 | | | 216,811 | | | (2) | % |
(a) The shift of some carrier arrangements from broker of record to fee-based BPO during 2024 impacted the growth in approved members as only broker of record arrangements are reflected in approved members. |
| | | | | | | | | | | | | | | | | |
| As of September 30, | | % Change |
| 2024 | | 2023 | |
Estimated Membership(5)(b) | | | | | |
Medicare(6) | | | | | |
| Medicare Advantage | 583,970 | | | 565,126 | | | 3 | % |
| Medicare Supplement | 95,153 | | | 93,732 | | | 2 | % |
| Medicare Part D | 194,303 | | | 209,475 | | | (7) | % |
| Total Medicare | 873,426 | | | 868,333 | | | 1 | % |
| | | | | |
| | | | | |
| | | | | |
Individual and Family(6) | 75,871 | | | 85,118 | | | (11) | % |
| | | | | |
| | | | | |
| | | | | |
| | | | | |
Ancillary(6) | 168,953 | | | 184,248 | | | (8) | % |
Small Business(7) | 41,172 | | | 46,316 | | | (11) | % |
| Total Estimated Membership | 1,159,422 | | | 1,184,015 | | | (2) | % |
(b) The shift of some carrier arrangements from broker of record to fee-based BPO during 2024 impacted the growth in estimated membership as only broker of record arrangements are reflected in estimated membership. |
______________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of GAAP Operating Costs and Expenses to Non-GAAP Operating Costs and Expenses(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | Nine Months Ended
September 30, |
| 2024 | | 2023 | | 2024 | | 2023 |
GAAP marketing and advertising expense(8) | $ | 29,665 | | | $ | 29,035 | | | $ | 95,185 | | | $ | 85,343 | |
Stock-based compensation expense | (437) | | | (605) | | | (1,792) | | | (1,598) | |
Non-GAAP marketing and advertising expense(1) | $ | 29,228 | | | $ | 28,430 | | | $ | 93,393 | | | $ | 83,745 | |
| | | | | | | |
GAAP customer care and enrollment expense(8) | $ | 39,321 | | | $ | 38,901 | | | $ | 100,773 | | | $ | 93,951 | |
| Stock-based compensation expense | (452) | | | (836) | | | (1,487) | | | (2,229) | |
Non-GAAP customer care and enrollment expense(1) | $ | 38,869 | | | $ | 38,065 | | | $ | 99,286 | | | $ | 91,722 | |
| | | | | | | |
GAAP technology and content expense(8) | $ | 12,264 | | | $ | 13,241 | | | $ | 38,613 | | | $ | 42,047 | |
| Stock-based compensation expense | (845) | | | (1,306) | | | (2,598) | | | (3,384) | |
Non-GAAP technology and content expense(1) | $ | 11,419 | | | $ | 11,935 | | | $ | 36,015 | | | $ | 38,663 | |
| | | | | | | |
GAAP general and administrative expense(8) | $ | 20,297 | | | $ | 22,937 | | | $ | 62,318 | | | $ | 72,310 | |
| Stock-based compensation expense | (2,745) | | | (3,807) | | | (9,248) | | | (10,530) | |
Non-GAAP general and administrative expense(1) | $ | 17,552 | | | $ | 19,130 | | | $ | 53,070 | | | $ | 61,780 | |
| | | | | | | |
| GAAP operating costs and expenses | $ | 101,608 | | | $ | 104,114 | | | $ | 306,298 | | | $ | 293,651 | |
| Stock-based compensation expense | (4,479) | | | (6,554) | | | (15,125) | | | (17,741) | |
| | | | | | | |
| | | | | | | |
| Impairment, restructuring and other charges | (61) | | | — | | | (9,409) | | | — | |
| | | | | | | |
Non-GAAP operating costs and expenses(1) | $ | 97,068 | | | $ | 97,560 | | | $ | 281,764 | | | $ | 275,910 | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
__________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of GAAP Net Loss Attributable to Common Stockholders to Adjusted EBITDA(1) (in thousands) and Adjusted EBITDA Margin(1):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | Nine Months Ended
September 30, |
| 2024 | | 2023 | | 2024 | | 2023 |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
GAAP net loss attributable to common stockholders | $ | (53,948) | | $ | (47,243) | | $ | (120,647) | | $ | (108,206) |
| Preferred stock dividends | 5,643 | | 5,320 | | 16,603 | | 15,644 |
| Change in preferred stock redemption value | 5,832 | | 4,898 | | 16,619 | | 12,158 |
| GAAP net loss | (42,473) | | (37,025) | | (87,425) | | (80,404) |
| Stock-based compensation expense | 4,479 | | 6,554 | | 15,125 | | 17,741 |
| | | | | | | |
| Depreciation and amortization | 3,827 | | 4,745 | | 12,511 | | 15,141 |
| | | | | | | |
| Impairment, restructuring and other charges | 61 | | — | | 9,409 | | — |
| | | | | | | |
| Interest expense | 2,859 | | 2,822 | | 8,517 | | 8,122 |
| Other income, net | (1,699) | | (2,684) | | (6,425) | | (7,500) |
Benefit from income taxes | (1,886) | | (2,509) | | (3,736) | | (8,660) |
Adjusted EBITDA(1) | $ | (34,832) | | $ | (28,097) | | $ | (52,024) | | $ | (55,560) |
Net loss margin | (73) | % | | (57) | % | | (40) | % | | (39) | % |
Adjusted EBITDA margin(1) | (60) | % | | (43) | % | | (24) | % | | (27) | % |
Reconciliation of GAAP Net Loss to Non-GAAP Net Loss(1) and GAAP Net Loss to Adjusted EBITDA Excluding Net Adjustment Revenue(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | $ Change | | % Change |
| 2024 | | 2023 | | |
GAAP net loss | $ | (42,473) | | | $ | (37,025) | | | $ | (5,448) | | (15)% |
Net adjustment revenue | (1,198) | | | (12,213) | | | | | |
Impairment, restructuring and other charges | 61 | | | — | | | | | |
Adjustment to benefit from income taxes, net | 284 | | | 2,935 | | | | | |
Non-GAAP net loss(1) | (43,326) | | | (46,303) | | | 2,977 | | 6% |
| Stock-based compensation expense | 4,479 | | | 6,554 | | | | | |
| | | | | | | |
| Depreciation and amortization | 3,827 | | | 4,745 | | | | | |
| | | | | | | |
| Interest expense | 2,859 | | | 2,822 | | | | | |
| Other income, net | (1,699) | | | (2,684) | | | | | |
| Adjustment to benefit from income taxes, net | (284) | | | (2,935) | | | | | |
| Benefit from income taxes | (1,886) | | | (2,509) | | | | | |
Adjusted EBITDA excluding net adjustment revenue(1) | $ | (36,030) | | | $ | (40,310) | | | $ | 4,280 | | 11% |
__________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of GAAP Total Revenue to Non-GAAP Total Revenue Excluding Net Adjustment Revenue(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | $ Change | | % Change |
| 2024 | | 2023 | | |
GAAP total revenue | $ | 58,409 | | | $ | 64,718 | | | $ | (6,309) | | | (10)% |
Net adjustment revenue | (1,198) | | | (12,213) | | | | | |
Non-GAAP total revenue excluding net adjustment revenue(1) | $ | 57,211 | | | $ | 52,505 | | | $ | 4,706 | | | 9% |
Reconciliation of Medicare Segment Revenue to Non-GAAP Medicare Segment Revenue(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | $ Change | | % Change |
| | 2024 | | 2023 | | |
Medicare segment revenue | $ | 53,221 | | | $ | 55,523 | | | $ | (2,302) | | | (4) | % |
Medicare net adjustment revenue | (1,090) | | | (9,291) | | | | | |
Non-GAAP Medicare segment revenue(1) | $ | 52,131 | | | $ | 46,232 | | | $ | 5,899 | | | 13 | % |
Reconciliation of E&I Segment Revenue to Non-GAAP E&I Segment Revenue(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | $ Change | | % Change |
| | 2024 | | 2023 | | |
E&I segment revenue | $ | 5,188 | | | $ | 9,195 | | | $ | (4,007) | | | (44) | % |
E&I net adjustment revenue | (108) | | | (2,922) | | | | | |
Non-GAAP E&I segment revenue(1) | $ | 5,080 | | | $ | 6,273 | | | $ | (1,193) | | | (19) | % |
Reconciliation of Segment Loss to Segment Loss Excluding Net Adjustment Revenue(1), Medicare Segment Loss to Medicare Segment Loss Excluding Net Adjustment Revenue(1) and E&I Segment Profit (Loss) to E&I Segment Profit (Loss) Excluding Net Adjustment Revenue(1) (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| Three Months Ended
September 30, | | $ Change | | % Change |
| | 2024 | | 2023 | | |
Segment loss(8) | $ | (18,732) | | | $ | (10,521) | | | $ | (8,211) | | | (78) | % |
Net adjustment revenue | (1,198) | | | (12,213) | | | | | |
Segment loss excluding net adjustment revenue(1) | $ | (19,930) | | | $ | (22,734) | | | $ | 2,804 | | | 12 | % |
| | | | | | | |
Medicare segment loss(8) | $ | (17,933) | | | $ | (15,331) | | | $ | (2,602) | | | (17) | % |
Medicare net adjustment revenue | (1,090) | | | (9,291) | | | | | |
Medicare segment loss excluding net adjustment revenue(1) | $ | (19,023) | | | $ | (24,622) | | | $ | 5,599 | | | 23 | % |
| | | | | | | |
E&I segment profit (loss)(8) | $ | (799) | | | $ | 4,810 | | | $ | (5,609) | | | (117) | % |
E&I net adjustment revenue | (108) | | | (2,922) | | | | | |
E&I segment profit (loss) excluding net adjustment revenue(1) | $ | (907) | | | $ | 1,888 | | | $ | (2,795) | | | (148) | % |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
__________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
RECONCILIATION OF GAAP TO NON-GAAP FINANCIAL MEASURES
(unaudited)
Reconciliation of Guidance GAAP Net Loss Attributable to Common Stockholders to Adjusted EBITDA(1) (in millions):
| | | | | | | | | | | |
| Full Year 2024 Guidance |
| Low | | High |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| | | |
| GAAP net loss attributable to common stockholders | $ | (81.5) | | | $ | (67.0) | |
| Impact from preferred stock | 45.0 | | | 45.0 | |
| GAAP net loss | (36.5) | | | (22.0) | |
| Stock-based compensation expense | 20.0 | | | 17.0 | |
| Depreciation and amortization | 19.0 | | | 18.0 | |
| Impairment, restructuring and other charges | 9.0 | | | 9.0 | |
| | | |
| Interest expense | 11.0 | | | 10.0 | |
| Other income, net | (8.0) | | | (9.0) | |
| Provision for (benefit from) income taxes | (7.0) | | | 2.0 | |
Adjusted EBITDA(1) | $ | 7.5 | | | $ | 25.0 | |
Reconciliation of Guidance GAAP Total Revenue to Guidance Non-GAAP Total Revenue Excluding Net Adjustment Revenue(1) (in millions):
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| Full Year 2024 Guidance | | | | Mid Guidance YoY |
| Low | | Mid | | High | | FY 2023 | | % Change |
GAAP total revenue | $ | 470.0 | | $ | 482.5 | | $ | 495.0 | | $ | 453.0 | | 7 | % |
Net adjustment revenue | (14.0) | | (17.0) | | (20.0) | | (48.0) | | |
Non-GAAP total revenue excluding net adjustment revenue(1) | $ | 456.0 | | $ | 465.5 | | $ | 475.0 | | $ | 405.0 | | 15 | % |
__________
Note: See accompanying footnotes on page 15.
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
(1)Non-GAAP Financial Information
This press release includes financial measures that are not calculated in accordance with U.S. generally accepted accounting principles (GAAP). To supplement eHealth’s condensed consolidated financial statements presented in accordance with GAAP, eHealth presents investors with non-GAAP financial measures, including non-GAAP total revenue excluding net adjustment revenue, non-GAAP operating costs and expenses, non-GAAP net income (loss), adjusted EBITDA, adjusted EBITDA margin, adjusted EBITDA excluding net adjustment revenue, non-GAAP Medicare segment revenue, non-GAAP E&I segment revenue, segment profit (loss) excluding net adjustment revenue, Medicare segment profit (loss) excluding net adjustment revenue and E&I segment profit (loss) excluding net adjustment revenue.
•Non-GAAP total revenue excluding net adjustment revenue is calculated by excluding the effect of net commission revenue from members approved in prior periods (“net adjustment revenue”) from total revenue.
•Non-GAAP operating costs and expenses are calculated by excluding the effect of expensing stock-based compensation related to stock options, restricted stock awards, performance-based and market-based awards and employee stock purchase plan from the respective GAAP operating costs and expenses. Total non-GAAP operating costs and expenses is calculated by excluding the effect of expensing stock-based compensation related to stock options, restricted stock awards, performance-based and market-based awards and employee stock purchase plan and impairment, restructuring and other charges from GAAP total operating costs and expenses.
•Non-GAAP net income (loss) is calculated by excluding net adjustment revenue and impairment, restructuring and other charges, net of tax from GAAP net income (loss).
•Adjusted EBITDA is calculated by excluding dividends for preferred stock and change in preferred stock redemption value (together the “impact from preferred stock”), provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles.
•Adjusted EBITDA margin is calculated as adjusted EBITDA divided by revenue.
•Adjusted EBITDA excluding net adjustment revenue is calculated by excluding net adjustment revenue, provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss).
•Non-GAAP Medicare segment revenue is calculated by excluding Medicare net adjustment revenue from Medicare segment revenue.
•Non-GAAP E&I segment revenue is calculated by excluding E&I net adjustment revenue from E&I segment revenue.
•Segment profit (loss) excluding net adjustment revenue is calculated by excluding net adjustment revenue from segment profit (loss).
•Medicare segment profit (loss) excluding net adjustment revenue is calculated by excluding Medicare net adjustment revenue from Medicare segment profit (loss).
•E&I segment profit (loss) excluding net adjustment revenue is calculated by excluding E&I net adjustment revenue from E&I segment profit (loss).
eHealth believes that the presentation of these non-GAAP financial measures provides important supplemental information to management and investors regarding financial and business trends relating to eHealth’s financial condition and results of operations. Management believes that the use of these non-GAAP financial measures provides consistency and comparability with eHealth’s past financial reports. Management also believes that the items described above provide an additional measure of eHealth’s operating results and facilitates comparisons of eHealth’s core operating performance against prior periods and business model objectives. This information is provided to investors in order to facilitate additional analyses of past, present and future operating performance and as a supplemental means to evaluate eHealth’s ongoing operations. eHealth believes that these non-GAAP financial measures are useful to investors in their assessment of eHealth’s operating performance.
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
Non-GAAP total revenue excluding net adjustment revenue, non-GAAP operating costs and expenses, non-GAAP net income (loss), adjusted EBITDA, adjusted EBITDA margin, adjusted EBITDA excluding net adjustment revenue, non-GAAP Medicare segment revenue, non-GAAP E&I segment revenue, segment profit (loss) excluding net adjustment revenue, Medicare segment profit (loss) excluding net adjustment revenue and E&I segment profit (loss) excluding net adjustment revenue are not calculated in accordance with GAAP, and should be considered supplemental to, and not as a substitute for, or superior to, financial measures calculated in accordance with GAAP. Non-GAAP financial measures used in this press release have limitations in that they do not reflect all of the revenue and costs associated with the operations of eHealth’s business and do not reflect income tax as determined in accordance with GAAP. As a result, you should not consider these measures in isolation or as a substitute for analysis of eHealth’s results as reported under GAAP. eHealth expects to continue to incur the stock-based compensation costs and depreciation and amortization described above, and exclusion of these costs, and their related income tax benefits, from non-GAAP financial measures should not be construed as an inference that these costs are unusual or infrequent. eHealth compensates for these limitations by prominently disclosing GAAP total revenue, GAAP net income (loss) before taxes, GAAP net income (loss), GAAP net income (loss) attributable to common stockholders, GAAP net income (loss) margin and providing investors with reconciliations from eHealth’s GAAP operating results to the non-GAAP financial measures for the relevant periods.
The tables above provide more details on the GAAP financial measures that are most directly comparable to the non-GAAP financial measures described above and the related reconciliations between these financial measures.
(2)Approved members represent the number of individuals on submitted applications that were approved by the relevant insurance carrier for the identified product during the current period for which we are the broker of record. The applications may be submitted in either the current period or prior periods. Not all approved members ultimately become paying members.
(3)Constrained lifetime value (“LTV”) of commissions per approved member for Medicare, individual and family and ancillary plans represents commissions estimated to be collected over the estimated life of an approved member’s plan after applying constraints in accordance with our revenue recognition policy. Constrained LTV of commissions per approved member for small business represents the estimated commissions we expect to collect from the plan over the following twelve months. The estimate is driven by multiple factors, including but not limited to, contracted commission rates, carrier mix, estimated average plan duration, the regulatory environment, and cancellations of insurance plans offered by health insurance carriers with which we have a relationship and applied constraints. The constraints are applied to help ensure that commissions estimated to be collected over the estimated life of an approved member’s plan are recognized as revenue only to the extent that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with future commissions receivable from the plan is subsequently resolved. These factors may result in varying values from period to period.
(4)Expense Metrics per Approved Member: Marketing initiatives are an important component of our strategy to increase revenue and are primarily designed to encourage consumers to complete an application for health insurance. We calculate and evaluate the customer care and enrollment (“CC&E”) expense per approved member and the variable marketing cost per approved member. We incur CC&E expenses in assisting applicants during the enrollment process. Variable marketing costs represent costs incurred in member acquisition from our direct marketing and marketing partner channels. Variable marketing costs exclude fixed overhead costs, such as personnel related costs, consulting expenses and other operating costs allocated to the marketing and advertising department.
The numerator used to calculate each member acquisition metric discussed above is the portion of the respective operating expenses for CC&E and marketing and advertising that is directly related to member acquisition for our sale of Medicare Advantage, Medicare Supplement and Medicare Part D prescription drug plans (collectively, the “Medicare Plans”) and for all individual and family major medical plans and short-term health insurance plans (collectively, “IFP Plans”), respectively, for which we are the broker of record. The denominator used to calculate each metric is based on a derived metric that represents the relative value of the new members acquired. For Medicare Plans, we call this derived metric Medicare Advantage (“MA”)-equivalent approved members, and for IFP Plans, we call this derived metric IFP-equivalent approved members. MA-equivalent approved members is a derived metric with a Medicare Part D approved member being weighted at 25% of a Medicare Advantage member and a Medicare Supplement member based on their relative LTVs at the time of our adoption of ASC 606. We calculate the number of MA-equivalent approved members by adding the total number of approved Medicare Advantage and Medicare Supplement members and 25% of the total number of approved Medicare Part D members during the periods presented. IFP-equivalent approved members is a derived metric with a short-term approved member being weighted at 33% of a major medical individual and family health insurance plan member based on their relative LTVs at the time of our adoption of ASC 606. We calculate the number of IFP-equivalent approved members by adding the total number of approved qualified and non-qualified health plan members and 33% of the total number of short-term approved members during the period presented.
(5)Estimated membership represents the estimated number of members active as of the date indicated based on the number of members for whom we have received or applied a commission payment during the period of estimation. There is generally up to a few months lag between newly approved plans and the receipt of commission payments from the health insurance carrier and is most pronounced in the fourth and first quarters of our fiscal year due to the annual enrollment period. A member who purchases and is active on multiple standalone insurance plans will be counted as a member more than once.
EHEALTH, INC.
Footnotes to Preceding Financial Statements and Metrics
Health insurance carriers bill and collect insurance premiums paid by our members. The carriers do not report to us the number of members that we have as of a given date. The majority of our members who terminate their policies do so by discontinuing their premium payments to the carrier or notifying the carrier directly and do not inform us of the cancellation. Also, some of our members pay their premiums less frequently than monthly. Given the number of months required to observe non-payment of commissions in order to confirm cancellations, we estimate the number of members who are active on insurance policies as of a specified date.
After we have estimated membership for a period, we may receive information from health insurance carriers that would have impacted the estimate if we had received the information prior to the date of estimation. We may receive commission payments or other information that indicates that a member who was not included in our estimates for a prior period was in fact an active member at that time, or that a member who was included in our estimates was in fact not an active member of ours. For instance, we reconcile information carriers provide to us and may determine that we were not historically paid commissions owed to us, which would cause us to have underestimated membership. Conversely, carriers may require us to return commission payments paid in a prior period due to policy cancellations for members we previously estimated as being active. We do not update our estimated membership numbers reported in previous periods. Instead, we reflect updated information regarding our historical membership in the membership estimate for the current period. If we experience a significant variance in historical membership as compared to our initial estimates, while we keep the prior period data consistent with previously reported amounts, we may provide the updated information in other communications or disclosures. As a result of the delay in our receipt of information from insurance carriers, actual trends in our membership are most discernible over periods longer than from one quarter to the next, making it difficult for us to determine with any certainty the impact of current conditions on our membership retention. Various circumstances could cause the assumptions and estimates that we make in connection with estimating our membership to be inaccurate, which would cause our membership estimates to be inaccurate.
(6)To estimate the number of members on Medicare-related, individual and family, and ancillary health insurance plans, we take the respective sum of (i) the number of members for whom we have received or applied a commission payment for a month that may be up to three months prior to the date of estimation (after reducing that number using historical experience for assumed member cancellations over the period being estimated); and (ii) the number of approved members over that period (after reducing that number using historical experience for an assumed number of members who do not accept their approved policy and for estimated member cancellations). To the extent we determine through confirmations from a health insurance carrier that a commission payment is delayed or is inaccurate as of the date of estimation, we adjust the estimated membership to also reflect the number of members for whom we expect to receive or to refund a commission payment. Further, to the extent we have received substantially all of the commission payments related to a given month during the period being estimated, we will take the number of members for whom we have received or applied a commission payment during the month of estimation. For ancillary health insurance plans, the one to three-month period varies by insurance product and is largely dependent upon the timeliness of commission payment and related reporting from the related carriers.
(7)To estimate the number of members on small business health insurance plans, we use the number of initial members at the time the group was approved, and we update this number for changes in membership if such changes are reported to us by the group or carrier. However, groups generally notify the carrier directly of policy cancellations and increases or decreases in group size without informing us. Health insurance carriers often do not communicate policy cancellation information or group size changes to us. We often are made aware of policy cancellations and group size changes at the time of annual renewal and update our membership statistics accordingly in the period they are reported.
(8)Beginning in the first quarter of 2024, primarily as a result of vacating excess office space, we modified our methodology used in allocating certain expenses for the purpose of evaluating financial and segment performance and resource allocation. Specifically, we no longer allocate our facilities-related expenses, and as a result, these costs are now reported within the “General and administrative” line in our Condensed Consolidated Statements of Comprehensive Loss and within Corporate for our segment profit (loss). We have recast the Condensed Consolidated Statements of Comprehensive Loss and our segment profit (loss) for the prior periods presented to conform to our current methodology. This resulted in a classification change of expenses from marketing and advertising, customer care and enrollment, and technology and content into general and administrative. Additionally, our segment profit (loss) no longer includes our facilities allocation to each of our segments and instead, these costs are included within Corporate. There was no impact to total operating costs and expenses, loss from operations, net loss or net loss per share attributable to common stockholders on our Condensed Consolidated Statements of Comprehensive Loss.

©2024 eHealthInsurance Services, Inc. Q3 2024 Financial Results 1

©2024 eHealthInsurance Services, Inc. 2 Safe Harbor Statement Forward-Looking Statements This presentation includes forward-looking statements within the meaning of the federal securities laws. Forward-looking statements generally relate to future events or our future financial or operating performance. Forward-looking statements in this presentation include, but are not limited to, the following: Medicare broker industry and broader Medicare market trends, our estimates regarding Medicare enrollment growth; our estimates regarding commissions receivable collection; our estimates of constrained lifetime value of commissions per approved member; our 2024 operational priorities, including our business and growth strategy, B2B strategy, local market strategy, product portfolio diversification, and member loyalty and retention strategy; our 2024 annual guidance for total revenue, GAAP net loss, adjusted EBITDA and operating cash flow; our estimates for positive net adjustment revenue and its expected impact on our 2024 annual guidance; the impact of our efforts to prepare for the annual enrollment period, our operational initiatives, including our Agency and Amplify fulfillment models, member retention initiatives and new platform features, and the expected impact of these initiatives on our business and financial results; our investments in technology, marketing , sales and operational initiatives and expected impact of these investments on conversions and our business; and other statements regarding our future operations, financial condition, prospects and business strategies. Our expectations and beliefs regarding these matters may not materialize, and actual results in future periods are subject to risks and uncertainties that could cause actual results to differ materially from those projected. These risks include those set forth in our filings with the Securities and Exchange Commission, including our latest Form 10-Q and 10-K. The forward-looking statements in this presentation are based on information available to us as of today, and we disclaim any obligation to update any forward-looking statements, except as required by law. Non-GAAP Information This presentation includes both GAAP and non-GAAP financial measures. The presentation of non-GAAP financial information is not intended to be considered in isolation or as a substitute for results prepared in accordance with GAAP. Definitions and reconciliations of the non-GAAP financial measures included in this presentation to the most directly comparable GAAP financial measures is available in the Appendix to this presentation. Management uses both GAAP and non-GAAP information in evaluating and operating its business internally and as such has determined that it is important to provide this information to investors.

©2024 eHealthInsurance Services, Inc. 3 Q3 2024 Earnings Highlights Q3 2024 Medicare submissions(1) across our core agency and carrier-dedicated Amplify platforms grew 22% compared to Q3 2023. Q3 2024 Medicare Advantage submissions(1) grew 26% compared to Q3 2023. Total Q3 2024 acquisition cost per MA-equivalent approved member declined 16% compared to Q3 2023. Q3 2024 total revenue was $58.4 million or a 10% year-over-year decline, driven by lower positive net adjustment revenue. Q3 2024 positive net adjustment revenue was $1.2 million compared to $12.2 million in Q3 of 2023. Q3 2024 Non-GAAP total revenue excluding net adjustment revenue(2) increased 9% year-over-year. Q3 2024 GAAP net loss was $42.5 million compared to Q3 2023 GAAP net loss of $37.0 million; Q3 2024 Non-GAAP net loss(2), which excludes the post-tax impact of positive net adjustment revenue and restructuring charges, improved 6% year-over-year. Q3 2024 adjusted EBITDA(2) was $(34.8) million compared to Q3 2023 adjusted EBITDA(1) of $(28.1) million; Q3 2024 adjusted EBITDA excluding net adjustment revenue(2) improved $4.3 million year-over-year driven primarily by Medicare Advantage approved member growth, improved Medicare acquisition costs and continued fixed cost reduction efforts. Successfully completed AEP preparations; achieved our licensed agent headcount targets and conducted a robust training program, developed our integrated brand marketing strategy and made further enhancements to our online platform. Third quarter results reflect strong Medicare enrollment growth and our investments in AEP preparedness (1) Submissions describe applications that are submitted by individuals online through our eHealth platform or completed with the assistance of our benefit advisors where the individual provides authorization to the benefit advisor to submit the application to the insurance carrier partner. The individual may have additional actions to take before the application will be reviewed by the insurance carrier and not all submissions ultimately become approved members. (2) Refer to the appendix for definitions of our non-GAAP financial measures and reconciliations to the most comparable GAAP measure.

©2024 eHealthInsurance Services, Inc. 4 AEP Preparation Highlights Marketing Effectiveness • Advancing our distinct consumer brand as an unbiased, transparent Medicare Matchmaker • Layer in messaging recognizing specifics of this AEP • Continue scaling high- performing direct branded channels • Prepared to drive higher quality, higher converting leads Omnichannel Differentiation • Continue to set ourselves apart with unique omnichannel enrollment tools: – MatchMonitor: ANOC review tool, walking beneficiaries through plan changes – LiveAdvise: video enrollment experience – Features such as licensed agent chat, co-browsing, and our proprietary plan recommendation algorithm – Complete end-to-end online shopping and enrollment Sales Excellence • Entered AEP fully prepared for significant increase in call volume that we anticipate • Successfully reached our hiring goals with an advisor mix that is more tenured relative to last year • Employing additional screeners, to improve customer experience and reduce wait times • Combination of training, advisor mix, and screening program is expected to elevate conversions Expanded our cross-functional member loyalty and retention program

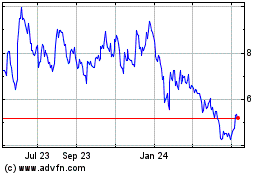
©2024 eHealthInsurance Services, Inc. 5 Q3 2024 Revenue Reflects Strong Medicare Performance and Lower Tail Revenue (1) Refer to the appendix for definitions of our non-GAAP financial measures and reconciliations to the most comparable GAAP measure. Total revenue in Q3 ‘24 declined 10% as a result of lower positive net adjustment (tail) revenue YoY, partially offset by our strong Medicare business performance. Non-GAAP total revenue excluding net adjustment revenue(1) increased 9% YoY Q3 ’24 total revenue also reflects non- commission revenue growth of 36% YoY reflecting continued scaling of Amplify fee- based BPO platform. $52.5 $57.2 $12.2 $1.2 Q3-FY23 Q3-FY24 Total Revenue ($MM) Non-GAAP total revenue ex. net adj. revenue Tail revenue(1) $58.4 $64.7 (10%) 9%

©2024 eHealthInsurance Services, Inc. 6 Q3 2024 Profitability Improved YoY Excluding Tail Revenue (1) Segment profit is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, and other income (expense), net. ($46.3) ($43.3) Q3-FY23 Q3-FY24 Non-GAAP Net Loss ($MM) ($40.3) ($36.0) Q3-FY23 Q3-FY24 Adjusted EBITDA ex. net adjustment revenue ($MM) Q3 ‘24 GAAP net loss was $42.5M compared to GAAP net loss of $37.0M in Q3 ‘23. Q3 ‘24 non-GAAP net loss(1) improved by $3.0M YoY reflecting increased application volume and favorable member acquisition costs. Q3 ‘24 adjusted EBITDA ex. net adjustment revenue(1) improved $4.3M YoY. (1) Refer to the appendix for definitions of our on-GAAP financi l measur s and reconciliatio s to the most co parable GAAP m asure. (1) ($37.0) ($42.5) Q3-FY23 Q3-FY24 GAAP Net Loss ($MM) ($28.1) ($34.8) Q3-FY23 Q3-FY24 Adjusted EBITDA ($MM) (1) (1)

©2024 eHealthInsurance Services, Inc. 7 Q3 2024 Medicare Segment Performance YoY comparisons of Medicare segment revenue and segment loss(1) were impacted by a decline in Medicare segment tail revenue. Q3 ‘24 Medicare segment revenue declined 4% YoY. Ex. tail, non-GAAP Medicare segment revenue(2) increased 13%. Q3 ‘24 Medicare segment loss(1) expanded 17% YoY. Q3 ‘24 Medicare segment loss excluding net adjustment revenue(2) improved 23% YoY. (1) Segment loss is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, interest expense and other income (expense), net. (2) Refer to the appendix for definitions of our non-GAAP financial measures and reconciliations to the most comparable GAAP measure. $46.2 $52.1 $9.3 $1.1 Q3-FY23 Q3-FY24 Medicare Segment Revenue ($MM) Medicare Segment Net Adjustment Revenue Non-GAAP Medicare Segment Revenue (4%) 13% $55.5 $53.2 ($15.3) ($17.9) Q3-FY23 Q3-FY24 Medicare Segment Loss(1)($MM) ($24.6) ($19.0) Q3-FY23 Q3-FY24 Medicare Segment Loss ex. Net Adjustment Revenue(2)($MM) (2)

©2024 eHealthInsurance Services, Inc. 8 Q3 2024 Medicare Segment Performance Cont. (1) Segment profit is calculated as total revenue for the applicable segment less direct and indirect allocated marketing and advertising, customer care and enrollment, technology and content and general and administrative operating expenses, excluding stock-based compensation expense, depreciation and amortization, impairment, restructuring and other charges, and other income (expense), net. $1,503 $1,256 Q3-FY23 Q3-FY24 Total Acquisition Cost per Medicare Advantage-equivalent Approved Member 45,400 55,518 Q3-FY23 Q3-FY24 Total Medicare Submissions(1) Q3 ’24 total Medicare submissions(1) grew 22% YoY. Acquisition cost per Medicare Advantage- equivalent approved member improved 16% YoY. (16%) 22% (1) Submissions describe applications that are submitted by individuals online through our eHealth platform or completed with the assistance of our benefit advisors where the individual provides authorization to the benefit advisor to submit the application to the insurance carrier partner. The individual may have additional actions to take before the application will be reviewed by the insurance carrier and not all submissions ultimately become approved members.

©2024 eHealthInsurance Services, Inc. Medicare Submitted Apps Growth 9 • eHealth generated strong YoY growth in third quarter MA submissions, across our agency and carrier- dedicated Amplify fulfillment models. • Medicare Supplement total submissions grew 5.2%; Med Supp BOR submission metrics reflect shift of one of our large partners to a carrier-dedicated BPO model. • Standalone Part D volumes continued to decline reflecting broader market trends. Total Submissions(1) Total BOR Submissions(1) Product Q3-2024 Q3-2023 YoY Q3-2024 Q3-2023 YoY Medicare Advantage 49,220 39,018 26.1% 47,002 38,934 20.7% Medicare Supplement 3,898 3,706 5.2% 1,728 3,706 (53.4%) Medicare Part D 2,400 2,676 (10.3%) 1,413 2,676 (47.2%) Total Medicare 55,518 45,400 22.3% 50,143 45,316 10.7% (1) Submissions describe applications that are submitted by individuals online through our eHealth platform or completed with the assistance of our benefit advisors where the individual provides authorization to the benefit advisor to submit the application to the insurance carrier partner. The individual may have additional actions to take before the application will be reviewed by the insurance carrier and not all submissions ultimately become approved members.

©2024 eHealthInsurance Services, Inc. Operating cash flow for the TTM ended 9/30/2024 declined year-over-year reflecting timing of certain cash receipts and cash compensation dynamics as we carried a larger advisor count this quarter than a year ago. 10 Cash Flow & Balance Sheet Highlights $8.1 ($24.1) TTM Sept 30, 2023 TTM Sept 30, 2024 Operating Cash Flow ($MM) $160.6 $117.8 Sept 30, 2023 Sept 30, 2024 Ending Cash, Cash Equivalents & Marketable Securities ($MM) $780.6 $814.0 Sept 30, 2023 Sept 30, 2024 Ending Commissions Receivable (Current & Non-Current) ($MM)

©2024 eHealthInsurance Services, Inc. 11 FY24 Operational Priorities Grow revenue year-over-year while producing positive adjusted EBITDA 1 Advance our local market focused, omni-channel enrollment engine to drive higher conversions and greater margins 2 Launch the next phase of our member loyalty & retention strategy 3 Drive our B2B strategy and fortify the organizational foundation that supports our strategic partners and direct- to-employer opportunities 4 Enhance eHealth’s comprehensive product portfolio beyond Medicare Advantage agency business to drive year-round growth 5

©2024 eHealthInsurance Services, Inc. 12 FY24 Guidance 2024 Full Year Guidance Guidance Range (in millions) Total Revenue $470 – $495 GAAP Net Income (Loss) ($36.5) – ($22) Adjusted EBITDA(1) $7.5 – $25 Operating Cash Flow ($10) – $0 We are reiterating the guidance ranges for FY 2024 that we updated as part of our last earnings report. Guidance includes an estimate for positive net adjustment revenue in the range of $14 to $20 million. (1) Refer to the appendix for definitions of our non-GAAP financial measures and reconciliations to the most comparable GAAP measure.

©2024 eHealthInsurance Services, Inc. Appendix 13

©2024 eHealthInsurance Services, Inc. 14 Non-GAAP Financial Measure Definitions Non-GAAP financial measures within this presentation are defined as follows: • Non-GAAP total revenue excluding net adjustment revenue is calculated by excluding the effect of net commission revenue from members approved in prior periods (“net adjustment revenue”) from total revenue. • Non-GAAP net income (loss) is calculated by excluding net adjustment revenue and impairment, restructuring and other charges, net of tax from GAAP net income (loss). • Adjusted EBITDA is calculated by excluding dividends for preferred stock and change in preferred stock redemption value (together the “impact from preferred stock”), provision for (benefit from) income taxes, depreciation and amortization, stock- based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss) attributable to common stockholders. Other non-recurring charges to GAAP net income (loss) attributable to common stockholders may include transaction expenses in connection with capital raising transactions (whether debt, equity or equity-linked) and acquisitions, whether or not consummated, purchase price adjustments and the cumulative effect of a change in accounting principles. • Adjusted EBITDA excluding net adjustment revenue is calculated by excluding net adjustment revenue, provision for (benefit from) income taxes, depreciation and amortization, stock-based compensation expense, impairment, restructuring and other charges, interest expense, other income (expense), net, and other non-recurring charges from GAAP net income (loss). • Non-GAAP Medicare segment revenue is calculated by excluding Medicare net adjustment revenue from Medicare segment revenue. • Medicare segment profit (loss) excluding net adjustment revenue is calculated by excluding Medicare net adjustment revenue from Medicare segment profit (loss).

©2024 eHealthInsurance Services, Inc. 15 Reconciliation of GAAP to Non-GAAP Financial Measures (1) See slide 14 for the definition of non-GAAP financial measures.

©2024 eHealthInsurance Services, Inc. 16 Reconciliation of GAAP to Non-GAAP Financial Measures (1) See slide 14 for the definition of non-GAAP financial measures.

©2024 eHealthInsurance Services, Inc. 17 Reconciliation of GAAP to Non-GAAP Financial Measures (1) See slide 14 for the definition of non-GAAP financial measures.

©2024 eHealthInsurance Services, Inc. 18 Reconciliation of Guidance GAAP to Non-GAAP Financial Measures (1) See slide 14 for the definition of non-GAAP financial measures.
v3.24.3
Cover Page
|
Nov. 06, 2024 |
| Cover [Abstract] |
|
| Document Type |
8-K
|
| Document Period End Date |
Nov. 06, 2024
|
| Entity Registrant Name |
EHEALTH, INC.
|
| Entity Incorporation, State or Country Code |
DE
|
| Entity File Number |
001-33071
|
| Entity Tax Identification Number |
56-2357876
|
| Entity Address, Address Line One |
13620 RANCH ROAD 620 N, SUITE A250
|
| Entity Address, City or Town |
AUSTIN
|
| Entity Address, State or Province |
TX
|
| Entity Address, Postal Zip Code |
78717
|
| City Area Code |
737
|
| Local Phone Number |
248-2340
|
| Written Communications |
false
|
| Soliciting Material |
false
|
| Pre-commencement Tender Offer |
false
|
| Title of 12(b) Security |
Common Stock, par value $0.001 per share
|
| Pre-commencement Issuer Tender Offer |
false
|
| Trading Symbol |
EHTH
|
| Security Exchange Name |
NASDAQ
|
| Entity Emerging Growth Company |
false
|
| Amendment Flag |
false
|
| Entity Central Index Key |
0001333493
|
| X |
- DefinitionBoolean flag that is true when the XBRL content amends previously-filed or accepted submission.
| Name: |
dei_AmendmentFlag |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionFor the EDGAR submission types of Form 8-K: the date of the report, the date of the earliest event reported; for the EDGAR submission types of Form N-1A: the filing date; for all other submission types: the end of the reporting or transition period. The format of the date is YYYY-MM-DD.
| Name: |
dei_DocumentPeriodEndDate |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:dateItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe type of document being provided (such as 10-K, 10-Q, 485BPOS, etc). The document type is limited to the same value as the supporting SEC submission type, or the word 'Other'.
| Name: |
dei_DocumentType |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:submissionTypeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionAddress Line 1 such as Attn, Building Name, Street Name
| Name: |
dei_EntityAddressAddressLine1 |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- Definition
+ References
+ Details
| Name: |
dei_EntityAddressCityOrTown |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCode for the postal or zip code
| Name: |
dei_EntityAddressPostalZipCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the state or province.
| Name: |
dei_EntityAddressStateOrProvince |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:stateOrProvinceItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionA unique 10-digit SEC-issued value to identify entities that have filed disclosures with the SEC. It is commonly abbreviated as CIK. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityCentralIndexKey |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:centralIndexKeyItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionIndicate if registrant meets the emerging growth company criteria. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityEmergingGrowthCompany |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionCommission file number. The field allows up to 17 characters. The prefix may contain 1-3 digits, the sequence number may contain 1-8 digits, the optional suffix may contain 1-4 characters, and the fields are separated with a hyphen.
| Name: |
dei_EntityFileNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:fileNumberItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTwo-character EDGAR code representing the state or country of incorporation.
| Name: |
dei_EntityIncorporationStateCountryCode |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarStateCountryItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe exact name of the entity filing the report as specified in its charter, which is required by forms filed with the SEC. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityRegistrantName |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionThe Tax Identification Number (TIN), also known as an Employer Identification Number (EIN), is a unique 9-digit value assigned by the IRS. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b-2
| Name: |
dei_EntityTaxIdentificationNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:employerIdItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionLocal phone number for entity.
| Name: |
dei_LocalPhoneNumber |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:normalizedStringItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 13e
-Subsection 4c
| Name: |
dei_PreCommencementIssuerTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14d
-Subsection 2b
| Name: |
dei_PreCommencementTenderOffer |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTitle of a 12(b) registered security. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection b
| Name: |
dei_Security12bTitle |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:securityTitleItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionName of the Exchange on which a security is registered. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 12
-Subsection d1-1
| Name: |
dei_SecurityExchangeName |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:edgarExchangeCodeItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as soliciting material pursuant to Rule 14a-12 under the Exchange Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Exchange Act
-Number 240
-Section 14a
-Subsection 12
| Name: |
dei_SolicitingMaterial |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionTrading symbol of an instrument as listed on an exchange.
| Name: |
dei_TradingSymbol |
| Namespace Prefix: |
dei_ |
| Data Type: |
dei:tradingSymbolItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
| X |
- DefinitionBoolean flag that is true when the Form 8-K filing is intended to satisfy the filing obligation of the registrant as written communications pursuant to Rule 425 under the Securities Act. Reference 1: http://www.xbrl.org/2003/role/presentationRef
-Publisher SEC
-Name Securities Act
-Number 230
-Section 425
| Name: |
dei_WrittenCommunications |
| Namespace Prefix: |
dei_ |
| Data Type: |
xbrli:booleanItemType |
| Balance Type: |
na |
| Period Type: |
duration |
|
eHealth (NASDAQ:EHTH)
Historical Stock Chart
From Nov 2024 to Dec 2024
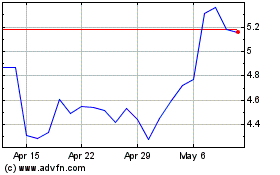
eHealth (NASDAQ:EHTH)
Historical Stock Chart
From Dec 2023 to Dec 2024