By Brent Kendall and Anna Wilde Mathews
The U.S. government is close to challenging two proposed mergers
between four of the nation's largest health-insurance companies,
according to people familiar with the matter, in what would
represent strong pushback against consolidation in the
industry.
The Justice Department as soon as this week could challenge
Anthem Inc.'s proposed acquisition of Cigna Corp. and Aetna Inc.'s
planned combination with Humana Inc. Antitrust lawsuits against the
planned mergers would be the culmination of concerns the Justice
Department has had about the deals from the outset. During a
yearlong review of the mergers, the department's skepticism hasn't
subsided, people familiar with the matter said.
The Wall Street Journal previously reported the mergers were in
trouble at the Justice Department, with antitrust enforcers worried
the deals would reduce competition and harm consumers.
The companies, however, have been given the chance to try to
persuade the department that any antitrust problems raised by the
deals could be addressed by shedding assets to competitors. The
department has been skeptical that asset sales, or divestitures,
would adequately preserve the current level of competition.
The government's firm stance is the latest sign that antitrust
enforcers, particularly in the late stages of the Obama
administration, are resisting large and potentially transformative
mergers in industries that already were becoming more
concentrated.
"Especially in this environment, we cannot afford to let up our
efforts, " Bill Baer, the acting associate attorney general, said
in a June speech. During a Senate hearing in March, Mr. Baer called
the insurance deals a "game-changer" that required close scrutiny
"to make sure we aren't making a mistake in which shareholders
benefit and the consumers pay the cost."
Bloomberg News first reported Tuesday that the department was
poised to file lawsuits this week or the next.
A Justice Department spokesman declined to comment.
An Aetna spokesman said the company "doesn't comment on rumors
and speculation, but we are steadfast in our belief that this deal
is good for consumers and the health-care system as a whole." The
Aetna spokesman said if the Justice Department does sue to block
its deal, the company would fight the suit.
Cigna and Anthem declined to comment. A Humana spokesman didn't
respond to a request for comment.
The deals were bold moves to reshape the top of the
health-insurance business, collapsing the top five companies in the
industry to three, each with annual revenue of more than $100
billion. Both combinations were unveiled last July, the culmination
of months of merger frenzy as the industry's biggest players
engaged in a chess-like series of moves and countermoves.
All of the merging companies argued they could achieve cost
savings and better results for customers with the scale that their
combinations would bring, amid changes and challenges tied to the
Affordable Care Act. They were also seeking to get closer to the
size and heft of the industry's largest player, UnitedHealth Group
Inc.
The two deals raised different antitrust concerns, however, and
legal challenges are likely to focus on distinct issues.
Anthem has previously told investors that it was likely to fight
if the Justice Department chose to sue, according to people with
knowledge of the matter, and Aetna has prepared a package of
divestitures that it has argued would remedy any competitive
concerns.
The Justice Department can't unilaterally block the deals. It
must convince a judge to do so.
The $48 billion Anthem-Cigna acquisition would create the
largest health insurer by enrollment, with more than 54 million
members, and $117 billion in annual revenue.
Justice Department officials have privately signaled major
concern about how the deal would affect the national employer
market, where the combination would shrink the number of
competitors to three from four. Other worries included the merger's
impact on individual insurance plans -- the coverage sold in the
exchanges that are at the heart of the Obama administration's
signature health law -- and on health-care providers, where a
combined insurer might have greater leverage in reimbursement
negotiations.
Anthem has argued the national-employer market is far more
complex, with sophisticated customers who often divvy up their
business. It has said the individual markets would remain
competitive, and that it wished to cooperate with health-care
providers.
With Aetna's $34 billion proposed acquisition of Humana, much of
the antitrust focus has been on private Medicare plans, Humana's
main business. An Aetna-Humana combination would become the biggest
seller of Medicare Advantage plans and have overall revenue of
about $115 billion based on 2015 totals.
Humana has a Medicare Advantage membership of about 3.19
million, or 17% of the national market, and Aetna has around 1.38
million, or 7%, according to Wells Fargo analysts. Among the areas
of greatest overlap are regions in Ohio, Florida and Missouri.
Missouri's insurance regulator has said the companies' combined
individual Medicare Advantage market share was more than 50%
statewide and above 90% in some counties.
Aetna has floated a package of Medicare Advantage assets,
attracting bids from major insurers. It also has said the full
competitive landscape for Medicare plans includes traditional
Medicare provided by the government.
If the deals do end up falling apart, all four companies will
remain considerably smaller than UnitedHealth.
Write to Brent Kendall at brent.kendall@wsj.com and Anna Wilde
Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
July 20, 2016 02:49 ET (06:49 GMT)
Copyright (c) 2016 Dow Jones & Company, Inc.
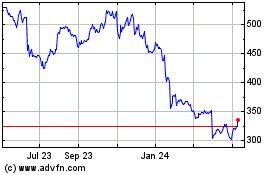
Humana (NYSE:HUM)
Historical Stock Chart
From Jun 2024 to Jul 2024
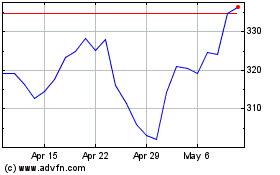
Humana (NYSE:HUM)
Historical Stock Chart
From Jul 2023 to Jul 2024