Company Announcement
- Full approval based on global Phase 3 study demonstrating
overall survival benefit of TIVDAK compared to
chemotherapy
- TIVDAK is the first antibody-drug conjugate in this patient
population to have positive overall survival data
Genmab A/S (Nasdaq: GMAB) and Pfizer Inc. (NYSE: PFE)
announced today the U.S. Food and Drug Administration (FDA) has
approved the supplemental Biologics License Application (sBLA) for
TIVDAK® (tisotumab vedotin-tftv) for the treatment of patients with
recurrent or metastatic cervical cancer with disease progression on
or after chemotherapy. This FDA action converts the September 2021
accelerated approval of TIVDAK to a full approval. TIVDAK is the
first antibody-drug conjugate (ADC) with demonstrated overall
survival data to be granted full FDA approval in this patient
population.
The approval is based on results from the global, randomized,
Phase 3 innovaTV 301 clinical trial (NCT04697628), in which TIVDAK
met its primary endpoint of overall survival (OS) in patients with
previously treated recurrent or metastatic cervical cancer compared
to chemotherapy. Secondary endpoints of progression-free survival
(PFS) and a confirmed objective response rate (ORR) were also met.
In October 2023, results from the innovaTV 301 study were initially
disclosed during the Presidential Symposium at the European Society
of Medical Oncology (ESMO) Congress.
“As a treating physician, it is encouraging to see overall
survival data among these patients and a manageable safety profile
with tisotumab vedotin,” said Brian Slomovitz, M.D., Director of
Gynecologic Oncology and Co-Chair of the Cancer Research Committee
at Mount Sinai Medical Center, Miami Beach. “Treatment options for
patients with advanced or recurrent cervical cancer are limited.
The five-year survival rate for patients who have metastatic
disease at diagnosis is less than 20% in the U.S.i There is a high
unmet need for more treatment options that have demonstrated
survival benefit in the contemporary treatment landscape. The
approval of tisotumab vedotin brings us a step closer to fulfilling
that need.”
The innovaTV 301 study met its primary endpoint of OS,
demonstrating a 30% reduction in the risk of death compared with
chemotherapy (Hazard ratio [HR]: 0.70 [95% CI: 0.54, 0.89],
two-sided p=0.0038ii). Median OS for patients treated with TIVDAK
was 11.5 months [95% CI: 9.8-14.9] versus chemotherapy 9.5 months
[95% CI: 7.9-10.7].
“The full FDA approval of TIVDAK represents a significant
achievement for women with recurrent and metastatic cervical
cancer, reinforcing TIVDAK as a treatment option that has proven to
extend survival in patients whose disease has advanced after
initial treatments,” said Jan van de Winkel, Ph.D., Chief Executive
Officer of Genmab. “This milestone underscores the importance of
our ongoing clinical development program to assess the full
potential of tisotumab vedotin as a treatment option in other
indications.”
"Recurrent or metastatic cervical cancer is a particularly
devastating and mostly incurable disease, and patients are in need
of survival-extending treatment options,” said Chris Boshoff, M.D.,
Ph.D., Chief Oncology Officer, Executive Vice President at Pfizer.
“Today’s full approval by the FDA reinforces the important role of
TIVDAK for these patients, as the first antibody-drug conjugate
with statistically significant prolonged overall survival
data.”
The U.S. Prescribing Information for TIVDAK includes a
BOXED WARNING for Ocular Toxicity as well as the
following Warnings and Precautions: peripheral neuropathy,
hemorrhage, pneumonitis, severe cutaneous adverse reactions, and
embryo-fetal toxicity. Please see below for additional
Important Safety Information.
The safety profile of TIVDAK in innovaTV 301 was consistent with
its known safety profile as presented in the U.S. prescribing
information. No new safety issues were identified. The most common
(≥25%) adverse reactions, including laboratory abnormalities, in
patients receiving TIVDAK were hemoglobin decreased (41%),
peripheral neuropathy (38%), conjunctival adverse reactions (37%),
aspartate aminotransferase increased (34%), nausea (33%), alanine
aminotransferase increased (30%), fatigue (28%), sodium decreased
(27%), epistaxis (26%), and constipation (25%).
The sBLA application received a Priority Review Designation,
which is granted by the U.S. FDA to medicines that may offer
significant advances in treatment or may provide a treatment where
no adequate therapy exists.iii TIVDAK was granted accelerated
approval in the U.S. by the FDA in September 2021, based on tumor
response and durability of response from the innovaTV 204 pivotal
Phase 2 single-arm clinical trial evaluating TIVDAK as a
monotherapy in patients with previously treated recurrent or
metastatic cervical cancer.
“Today marks a great day for patients, especially adults
battling advanced cervical cancer,” said Tamika Felder, cervical
cancer patient advocate and Founder and Chief Visionary Officer,
Cervivor, Inc. “This full approval opens up new treatment paths for
this patient community who have long faced limited options.”
About Cervical Cancer Cervical cancer remains a disease with
high unmet need despite advances in effective vaccination and
screening practices to prevent and diagnose pre-/early-stage
cancers for curative treatment. Recurrent and/or metastatic
cervical cancer is a particularly devastating and mostly incurable
disease; up to 15% of adults with cervical cancer present with
metastatic disease at diagnosisiv,v and, for adults diagnosed at
earlier stages who receive treatment, up to 61%vi will experience
disease recurrence. It was estimated that in 2023, more than 13,960
new cases of invasive cervical cancer were diagnosed in the U.S.
and 4,310 adults would die from the disease.vii
About the innovaTV 301 Trial The innovaTV 301 trial
(NCT04697628) is a global, 1:1 randomized, open-label Phase 3 trial
evaluating TIVDAK® (tisotumab vedotin-tftv) versus investigator’s
choice of single agent chemotherapy (topotecan, vinorelbine,
gemcitabine, irinotecan or pemetrexed) in 502 patients with
recurrent or metastatic cervical cancer who received one or two
prior systemic regimens in the recurrent or metastatic setting.
Patients with recurrent or metastatic cervical cancer with
squamous cell, adenocarcinoma or adenosquamous histology, and
disease progression during or after treatment with chemotherapy
doublet +/- bevacizumab and an anti-PD-(L)1 agent (if eligible) are
included. The primary endpoint was overall survival. The main
secondary outcomes were progression-free survival and objective
response rate.
The study was conducted by Seagen, which was acquired by Pfizer
in December 2023, in collaboration with Genmab, European Network of
Gynaecological Oncological Trial Groups (ENGOT, study number ENGOT
cx-12) and the Gynecologic Oncology Group (GOG) Foundation (study
number GOG 3057), as well as other global gynecological oncology
cooperative groups. For more information about the Phase 3 innovaTV
301 clinical trial and other clinical trials with tisotumab
vedotin, please visit www.clinicaltrials.gov.
About TIVDAK® (tisotumab vedotin-tftv) TIVDAK (tisotumab
vedotin-tftv) is an antibody-drug conjugate (ADC) composed of
Genmab’s human monoclonal antibody directed to tissue factor (TF)
and Pfizer’s ADC technology that utilizes a protease-cleavable
linker that covalently attaches the microtubule-disrupting agent
monomethyl auristatin E (MMAE) to the antibody. Nonclinical data
suggest that the anticancer activity of tisotumab vedotin-tftv is
due to the binding of the ADC to TF-expressing cancer cells,
followed by internalization of the ADC-TF complex and release of
MMAE via proteolytic cleavage. MMAE disrupts the microtubule
network of actively dividing cells, leading to cell cycle arrest
and apoptotic cell death. In vitro, tisotumab vedotin-tftv also
mediates antibody-dependent cellular phagocytosis and
antibody-dependent cellular cytotoxicity.
Indication TIVDAK is indicated for the treatment of adult
patients with recurrent or metastatic cervical cancer (r/mCC) with
disease progression on or after chemotherapy.
Important Safety Information
BOXED WARNING: OCULAR TOXICITY
TIVDAK can cause severe ocular toxicities resulting in changes
in vision, including severe vision loss, and corneal ulceration.
Conduct an ophthalmic exam, including an assessment of ocular
symptoms, visual acuity, and slit lamp exam of the anterior segment
of the eye prior to initiation of TIVDAK, prior to every cycle for
the first nine cycles, and as clinically indicated. Adhere to the
required premedication and eye care before, during, and after
infusion. Withhold TIVDAK until improvement and resume, reduce the
dose, or permanently discontinue, based on severity.
Warnings and Precautions
Ocular adverse reactions: TIVDAK can cause severe ocular adverse
reactions, including conjunctivitis, keratopathy (keratitis,
punctate keratitis, and ulcerative keratitis), and dry eye
(increased lacrimation, eye pain, eye discharge, pruritus,
irritation, and foreign body sensation), that may lead to changes
in vision and/or corneal ulceration.
Ocular adverse reactions occurred in 55% of patients with
cervical cancer treated with TIVDAK across clinical trials. The
most common were conjunctivitis (32%), dry eye (24%), keratopathy
(17%), and blepharitis (5%). Grade 3 ocular adverse reactions
occurred in 3.3% of patients, including severe ulcerative keratitis
in 1.2% of patients. Nine patients (2.1%) experienced ulcerative
keratitis (including one with perforation requiring corneal
transplantation), six (1.4%) conjunctival ulcer, four (0.9%)
corneal erosion, two (0.5%) conjunctival erosion, and two (0.5%)
symblepharon.
In innovaTV 301, 8 patients (3.2%) experienced delayed ocular
adverse reactions occurring more than 30 days after discontinuation
of TIVDAK. These adverse reactions included 3 patients with
ulcerative keratitis, and one patient (each) with keratitis,
punctate keratitis and corneal erosion, blepharitis and
conjunctival hyperemia, conjunctival scar, and conjunctivitis and
xerophthalmia.
Refer patients to an eye care provider to conduct an ophthalmic
exam prior to initiation of TIVDAK, prior to every cycle for the
first nine cycles, and as clinically indicated. The exam should
include visual acuity, slit lamp exam of the anterior segment of
the eye, and an assessment of normal eye movement and ocular signs
or symptoms which include dry or irritated eyes, eye secretions, or
blurry vision.
Adhere to the required premedication and eye care before,
during, and after infusion to reduce the risk of ocular adverse
reactions. Monitor for ocular toxicity and promptly refer patients
to an eye care provider for any new or worsening ocular signs and
symptoms. Withhold, reduce, or permanently discontinue TIVDAK based
on the severity or persistence of the ocular adverse reaction.
Peripheral Neuropathy (PN) occurred in 39% of cervical
cancer patients treated with TIVDAK across clinical trials; 6% of
patients experienced Grade 3 PN. PN adverse reactions included
peripheral sensory neuropathy (23%), PN (5%), paresthesia (3.8%),
peripheral sensorimotor neuropathy (3.3%), muscular weakness
(2.8%), and peripheral motor neuropathy (2.4%). One patient with
another tumor type treated with TIVDAK at the recommended dose
developed Guillain- Barre syndrome.
Monitor patients for signs and symptoms of neuropathy such as
paresthesia, tingling or a burning sensation, neuropathic pain,
muscle weakness, or dysesthesia. For new or worsening PN, withhold,
then dose reduce, or permanently discontinue TIVDAK based on the
severity of PN.
Hemorrhage occurred in 51% of cervical cancer patients treated
with TIVDAK across clinical trials. The most common all grade
hemorrhage adverse reaction was epistaxis (33%). Grade 3 hemorrhage
occurred in 4% of patients.
Monitor patients for pulmonary symptoms of pneumonitis. Symptoms
may include hypoxia, cough, dyspnea or interstitial infiltrates on
radiologic exams. Infectious, neoplastic, and other causes for such
symptoms should be excluded through appropriate investigations.
Withhold TIVDAK for patients who develop persistent or recurrent
Grade 2 pneumonitis and consider dose reduction. Permanently
discontinue TIVDAK in all patients with Grade 3 or 4
pneumonitis.
Pneumonitis that is severe, life-threatening, or fatal can occur
in patients treated with antibody-drug conjugates containing
vedotin, including TIVDAK. Among cervical cancer patients treated
with TIVDAK across clinical trials, 4 patients (0.9%) experienced
pneumonitis, including 1 patient who had a fatal outcome.
Monitor patients for pulmonary symptoms of pneumonitis. Symptoms
may include hypoxia, cough, dyspnea or interstitial infiltrates on
radiologic exams. Infectious, neoplastic, and other causes for
symptoms should be excluded through appropriate investigations.
Withhold TIVDAK for patients who develop persistent or recurrent
Grade 2 pneumonitis and consider dose reduction. Permanently
discontinue TIVDAK in all patients with Grade 3 or 4
pneumonitis.
Severe cutaneous adverse reactions (SCAR), including events of
fatal or life-threatening Stevens-Johnson syndrome (SJS), can occur
in patients treated with TIVDAK. SCAR occurred in 1.6% of cervical
cancer patients treated with TIVDAK across clinical trials. Grade
≥3 SCAR occurred in 0.5% of patients, including 1 patient who had a
fatal outcome.
Monitor patients for signs or symptoms of SCAR, which include
target lesions, worsening skin reactions, blistering or peeling of
the skin, painful sores in mouth, nose, throat, or genital area,
fever or flu-like symptoms, and swollen lymph nodes. If signs or
symptoms of SCAR occur, withhold TIVDAK until the etiology of the
reaction has been determined. Early consultation with a specialist
is recommended to ensure greater diagnostic accuracy and
appropriate management. Permanently discontinue TIVDAK for
confirmed Grade 3 or 4 SCAR, including SJS.
Embryo-fetal toxicity: TIVDAK can cause fetal harm when
administered to a pregnant woman. Advise patients of the potential
risk to a fetus. Advise females of reproductive potential to use
effective contraception during treatment with TIVDAK and for 2
months after the last dose. Advise male patients with female
partners of reproductive potential to use effective contraception
during treatment with TIVDAK and for 4 months after the last
dose.
Adverse Reactions
Across clinical trials of TIVDAK in 425 patients with r/mCC, the
most common (≥25%) adverse reactions, including laboratory
abnormalities, were hemoglobin decreased (45%), PN (39%),
conjunctival adverse reactions (38%), nausea (37%), fatigue (36%),
aspartate aminotransferase increased (33%), epistaxis (33%),
alopecia (31%), alanine aminotransferase increased (30%), and
hemorrhage (28%).
innovaTV 301 Study: 250 patients with r/mCC with disease
progression on or after systemic therapy
Serious adverse reactions occurred in 33% of patients
receiving TIVDAK; the most common (≥2%) were urinary tract
infection (4.8%), small intestinal obstruction (2.4%), sepsis,
abdominal pain, and hemorrhage (each 2%). Fatal adverse
reactions occurred in 1.6% of patients who received TIVDAK,
including acute kidney injury, pneumonia, sepsis, and SJS (each
0.4%).
Adverse reactions leading to permanent discontinuation
occurred in 15% of patients receiving TIVDAK; the most common (≥3%)
were PN and ocular adverse reactions (each 6%). Adverse
reactions leading to dose interruption occurred in 39% of
patients receiving TIVDAK; the most common (≥3%) were ocular
adverse reactions (16%) and PN (6%). Adverse reactions leading
to dose reduction occurred in 30% of patients receiving TIVDAK;
the most common (≥3%) were PN and ocular adverse reactions (each
10%). The ocular adverse reactions included conjunctival disorders
(4.8%), keratopathy (4%), and dry eye (0.8%).
innovaTV 204 Study: 101 patients with r/mCC with disease
progression on or after chemotherapy
Serious adverse reactions occurred in 43% of patients;
the most common (≥3%) were ileus (6%), hemorrhage (5%), pneumonia
(4%), PN, sepsis, constipation, and pyrexia (each 3%). Fatal
adverse reactions occurred in 4% of patients who received
TIVDAK, including septic shock, pneumonitis, sudden death, and
multisystem organ failure (each 1%).
Adverse reactions leading to permanent discontinuation
occurred in 13% of patients receiving TIVDAK; the most common (≥3%)
were PN (5%) and corneal adverse reactions (4%). Adverse
reactions leading to dose interruption occurred in 47% of
patients; the most common (≥3%) were PN (8%), conjunctival adverse
reactions, and hemorrhage (each 4%). Adverse reactions leading
to dose reduction occurred in 23% of patients; the most common
(≥3%) were conjunctival adverse reactions (9%) and corneal adverse
reactions (8%).
Drug Interactions
Strong CYP3A4 inhibitors: Concomitant use with strong CYP3A4
inhibitors may increase unconjugated monomethyl auristatin E (MMAE)
exposure, which may increase the risk of TIVDAK adverse reactions.
Closely monitor patients for TIVDAK adverse reactions.
Use in Specific Populations
Moderate or severe hepatic impairment: MMAE exposure and adverse
reactions are increased. Avoid use.
Lactation: Advise lactating women not to breastfeed during
TIVDAK treatment and for at least 3 weeks after the last dose.
Please see full prescribing information, including BOXED WARNING
for TIVDAK here.
About Genmab Genmab is an international biotechnology
company with a core purpose guiding its unstoppable team to strive
towards improving the lives of patients through innovative and
differentiated antibody therapeutics. For 25 years, its passionate,
innovative and collaborative team has invented next-generation
antibody technology platforms and leveraged translational,
quantitative, and data sciences, resulting in a proprietary
pipeline including bispecific T-cell engagers, next-generation
immune checkpoint modulators, effector function enhanced
antibodies, and antibody-drug conjugates. To help develop and
deliver novel antibody therapies to patients, Genmab has formed 20+
strategic partnerships with biotechnology and pharmaceutical
companies. By 2030, Genmab’s vision is to transform the lives of
people with cancer and other serious diseases with
knock-your-socks-off (KYSO®) antibody medicines.
Established in 1999, Genmab is headquartered in Copenhagen,
Denmark with locations in Utrecht, the Netherlands, Princeton, New
Jersey, U.S., and Tokyo, Japan. For more information, please visit
Genmab.com and follow us on LinkedIn and X.
About Pfizer Oncology At Pfizer Oncology, we are at the
forefront of a new era in cancer care. Our industry-leading
portfolio and extensive pipeline includes game-changing mechanisms
of action to attack cancer from multiple angles, including
antibody-drug conjugates (ADCs), small molecules, bispecific
antibodies and other immunotherapy biologics. We are focused on
delivering transformative therapies in some of the world’s most
common cancers, including breast cancer, genitourinary cancer,
hematology-oncology and thoracic cancers, which includes lung
cancer. Driven by science, we are committed to accelerating
breakthroughs to extend and improve patients’ lives.
About the Pfizer and Genmab Collaboration Tisotumab vedotin is
co-owned by Genmab and Pfizer, under an agreement in which the
companies share costs and profits for the product on a 50:50
basis.
Genmab Forward Looking Statements This Company Announcement
contains forward looking statements. The words “believe”, “expect”,
“anticipate”, “intend” and “plan” and similar expressions identify
forward looking statements. Actual results or performance may
differ materially from any future results or performance expressed
or implied by such statements. The important factors that could
cause our actual results or performance to differ materially
include, among others, risks associated with pre-clinical and
clinical development of products, uncertainties related to the
outcome and conduct of clinical trials including unforeseen safety
issues, uncertainties related to product manufacturing, the lack of
market acceptance of our products, our inability to manage growth,
the competitive environment in relation to our business area and
markets, our inability to attract and retain suitably qualified
personnel, the unenforceability or lack of protection of our
patents and proprietary rights, our relationships with affiliated
entities, changes and developments in technology which may render
our products or technologies obsolete, and other factors. For a
further discussion of these risks, please refer to the risk
management sections in Genmab’s most recent financial reports,
which are available on www.genmab.com and the risk factors included
in Genmab’s most recent Annual Report on Form 20-F and other
filings with the U.S. Securities and Exchange Commission (SEC),
which are available at www.sec.gov. Genmab does not undertake any
obligation to update or revise forward looking statements in this
Company Announcement nor to confirm such statements to reflect
subsequent events or circumstances after the date made or in
relation to actual results, unless required by law.
Genmab A/S and/or its subsidiaries own the following trademarks:
Genmab®; the Y-shaped Genmab logo®; Genmab in combination with the
Y-shaped Genmab logo®; HuMax®; DuoBody®; HexaBody®; DuoHexaBody®
and HexElect®. Tivdak® is a trademark of Pfizer Inc.
Pfizer Disclosure Notice The information contained in this
release is as of April 29, 2024. Pfizer assumes no obligation to
update forward-looking statements contained in this release as the
result of new information or future events or developments.
This release contains forward-looking information about Pfizer
Oncology and TIVDAK® (tisotumab vedotin-tftv), including its
potential benefits and its ongoing clinical development program,
that involves substantial risks and uncertainties that could cause
actual results to differ materially from those expressed or implied
by such statements. Risks and uncertainties include, among other
things, uncertainties regarding the commercial success of TIVDAK;
the uncertainties inherent in research and development, including
the ability to meet anticipated clinical endpoints, commencement
and/or completion dates for our clinical trials, regulatory
submission dates, regulatory approval dates and/or launch dates, as
well as the possibility of unfavorable new clinical data and
further analyses of existing clinical data; the risk that clinical
trial data are subject to differing interpretations and assessments
by regulatory authorities; whether regulatory authorities will be
satisfied with the design of and results from our clinical studies;
whether and when drug applications may be filed in particular
jurisdictions for TIVDAK; whether and when any applications that
may be pending or filed for TIVDAK may be approved by regulatory
authorities, which will depend on myriad factors, including making
a determination as to whether the product’s benefits outweigh its
known risks and determination of the product’s efficacy and, if
approved, whether TIVDAK will be commercially successful; decisions
by regulatory authorities impacting labeling, manufacturing
processes, safety and/or other matters that could affect the
availability or commercial potential of TIVDAK; whether the
collaboration between Pfizer and Genmab will be successful;
uncertainties regarding the impact of COVID-19 on Pfizer’s
business, operations and financial results; and competitive
developments.
A further description of risks and uncertainties can be found in
Pfizer’s Annual Report on Form 10-K for the fiscal year ended
December 31, 2023 and in its subsequent reports on Form 10-Q,
including in the sections thereof captioned “Risk Factors” and
“Forward-Looking Information and Factors That May Affect Future
Results”, as well as in its subsequent reports on Form 8-K, all of
which are filed with the U.S. Securities and Exchange Commission
and available at www.sec.gov and www.pfizer.com.
i Cervical Cancer: Statistics. American Society of Clinical
Oncology (ASCO). September 2023.
https://www.cancer.net/cancer-types/cervical-cancer/statistics ii
The threshold for statistical significance is 0.0226 (two-sided).
iii Priority Review. U.S. Food and Drug Administration. January 4,
2018.
https://www.fda.gov/patients/fast-track-breakthrough-therapy-accelerated-approval-priority-review/priority-review
iv National Cancer Institute. SEER Cancer Stat Facts: Cervical
Cancer. 2023. https://seer.cancer.gov/statfacts/html/cervix.html v
McLachlan J, Boussios S, Okines A, et al. The impact of systemic
therapy beyond first-line treatment for advanced cervical cancer.
Clin Oncol (R Coll Radiol). 2017;29(3):153-60. vi Pfaendler KS,
Tewari KS. Changing paradigms in the systemic treatment of advanced
cervical cancer. Am J Obstet Gynecol. 2016 Jan;214(1):22-30. doi:
10.1016/j.ajog.2015.07.022. Epub 2015 Jul 26. PMID: 26212178;
PMCID: PMC5613936. vii Key Statistics for Cervical Cancer. American
Cancer Society. Atlanta, GA. 2023.
https://www.cancer.org/cancer/types/cervical-cancer/about/key-statistics.html
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240422914519/en/
Investor and Media Contacts:
Genmab A/S Contacts: For Media: Marisol Peron,
Senior Vice President, Global Communications & Corporate
Affairs T: +1 (609) 524-0065; E: mmp@genmab.com
For Investor Relations: Andrew Carlsen, Vice President, Head of
Investor Relations T: +45 3377-9558; E: acn@genmab.com
Pfizer Contacts: For Media:
PfizerMediaRelations@Pfizer.com +1 (212) 733-1226
For Investor Relations: IR@Pfizer.com +1 (212) 733-4848
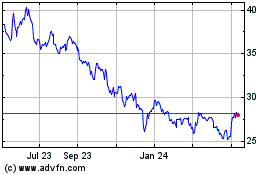
Pfizer (NYSE:PFE)
Historical Stock Chart
From Feb 2025 to Mar 2025
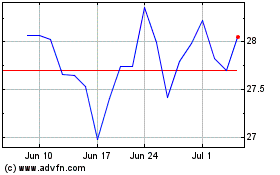
Pfizer (NYSE:PFE)
Historical Stock Chart
From Mar 2024 to Mar 2025