- Enfortumab vedotin plus pembrolizumab continues to demonstrate
superior efficacy versus chemotherapy in a broad population,
reinforcing the combination as standard of care in first-line
treatment of la/mUC
- At nearly 30 months of follow-up in the Phase 3 EV-302 trial,
the combination doubled median overall survival and
progression-free survival compared to chemotherapy, with no new
safety signals identified
Pfizer Inc. (NYSE: PFE) and Astellas Pharma Inc. (TSE: 4503,
President and CEO: Naoki Okamura, “Astellas”) today announced
additional follow-up results from the Phase 3 EV-302 clinical trial
(also known as KEYNOTE-A39) evaluating the efficacy and safety of
PADCEV ® (enfortumab vedotin-ejfv), a Nectin-4 directed
antibody-drug conjugate, plus KEYTRUDA® (pembrolizumab), a PD-1
inhibitor, in patients with previously untreated locally advanced
or metastatic urothelial cancer (la/mUC). The results showed a
sustained overall survival (OS) and progression-free survival (PFS)
benefit consistent with the findings of the primary analysis after
an additional 12 months of follow-up (median follow-up of 29.1
months).1,2 These data will be presented during a rapid oral
session (Abstract 664) at the American Society of Clinical Oncology
Genitourinary Cancers Symposium (ASCO GU) 2025 in San Francisco,
CA, on February 14 at 4:10pm PT.
This press release features multimedia. View
the full release here:
https://www.businesswire.com/news/home/20250210184062/en/
Thomas Powles, M.R.C.P., M.D., Professor of Genitourinary
Oncology at Queen Mary University of London; Director, Barts Cancer
Center, London; EV-302 Primary Investigator
“These latest findings from the EV-302 trial reaffirm the
primary results, which demonstrated survival improvements for
patients treated with enfortumab vedotin and pembrolizumab that
were previously unprecedented in locally advanced or metastatic
urothelial cancer. These data show that the potential survival
benefit has become even more robust with extended follow up and
further solidify the combination as standard of care.”
Results showed enfortumab vedotin plus pembrolizumab reduced the
risk of death by 49% versus chemotherapy (hazard ratio [HR] = 0.51,
95% confidence interval [CI], 0.43-0.61). The median OS was 33.8
months for the combination versus 15.9 months for chemotherapy. The
OS benefit was observed in all prespecified subgroups, including
cisplatin eligible and ineligible subgroups. Enfortumab vedotin
plus pembrolizumab also reduced the risk of disease progression or
death by 52% versus chemotherapy (HR = 0.48, 95% CI, 0.41-0.57).
The median PFS was 12.5 months for the combination versus 6.3
months for chemotherapy. The safety profile was consistent with
previous findings and no new safety concerns were identified.1
Please see Important Safety Information at the end of this press
release, including BOXED WARNING for enfortumab vedotin.
In addition to longer follow-up data, an exploratory analysis
evaluating treatment outcomes and safety profile in patients with
confirmed complete response (cCR) will also be presented. Among
patients evaluable for response, confirmed objective response rate
(cORR) was 67.5% for enfortumab vedotin plus pembrolizumab compared
to 44.2% for chemotherapy. Median duration of response (DOR) was
23.3 months (95% CI, 17.8-not estimable [NE]) for the combination
and 7.0 months (95% CI, 6.2-9.0) for chemotherapy. A cCR was
achieved in 30.4% of patients treated with enfortumab vedotin plus
pembrolizumab and 14.5% of patients treated with chemotherapy.
Median duration of cCR was not reached for the combination and 15.2
months (95% CI, 10.3-NE) for chemotherapy. In patients with cCR,
grade ≥3 treatment-related adverse events occurred in 61.7% of
patients in the enfortumab vedotin plus pembrolizumab arm compared
to 71.9% in the chemotherapy arm. There were no treatment-related
deaths in the cCR subgroup.1
Roger Dansey, M.D., Chief Oncology Officer, Pfizer
“Patients with bladder cancer can face a poor prognosis,
particularly in the advanced stages, and until recently had few
available treatment options. The updated EV-302 results show
sustained long-term efficacy in a broad population that includes
both cisplatin eligible and ineligible patients and reinforce this
combination’s ability to reshape the urothelial cancer treatment
landscape.”
Ahsan Arozullah, M.D., M.P.H., Senior Vice President, Head of
Oncology Development, Astellas
“The combination of enfortumab vedotin and pembrolizumab was the
first approval to offer an alternative to platinum-containing
chemotherapy, which had been the standard of care for first-line
locally advanced or metastatic urothelial cancer for decades. We
are delighted that the additional follow-up results of the EV-302
trial show a durable benefit. These data represent yet another
milestone in our long-standing commitment to helping patients
around the world live longer and healthier lives.”
Enfortumab vedotin plus pembrolizumab is approved for the
treatment of adult patients with la/mUC in the United States, the
European Union, Japan and a number of other countries around the
world. Enfortumab vedotin is also approved as a single agent for
the treatment of adult patients with la/mUC who have previously
received a PD-1/PD-L1 inhibitor and platinum-containing
chemotherapy or are ineligible for cisplatin-containing
chemotherapy and have previously received one or more prior lines
of therapy.3
+++
About EV-302
The EV-302 trial is an open-label, randomized, controlled Phase
3 study, evaluating enfortumab vedotin in combination with
pembrolizumab versus platinum-containing chemotherapy in patients
with previously untreated la/mUC. The study enrolled 886 patients
with previously untreated la/mUC who were eligible for cisplatin-
or carboplatin-containing chemotherapy regardless of PD-L1 status.
Patients were randomized to receive either enfortumab vedotin in
combination with pembrolizumab or platinum-containing chemotherapy.
The dual primary endpoints of this trial are OS and PFS per RECIST
v1.1 by blinded independent central review (BICR). Select secondary
endpoints include ORR per RECIST v1.1 by BICR, DOR per RECIST v1.1
by BICR, and safety.4
The EV-302 trial is part of an extensive clinical program
evaluating this combination in multiple stages of urothelial cancer
and other solid tumors. Primary results from the EV-302 study were
presented at the European Society for Medical Oncology (ESMO)
Congress in October 2023.
About PADCEV® (enfortumab vedotin-ejfv)
PADCEV ® (enfortumab vedotin-ejfv) is a first-in-class
antibody-drug conjugate (ADC) that is directed against Nectin-4, a
protein located on the surface of cells and highly expressed in
bladder cancer.5 Nonclinical data suggest the anticancer activity
of enfortumab vedotin is due to its binding to Nectin-4-expressing
cells, followed by the internalization and release of the
anti-tumor agent monomethyl auristatin E (MMAE) into the cell,
which result in the cell not reproducing (cell cycle arrest) and in
programmed cell death (apoptosis).3
PADCEV ® (enfortumab vedotin-ejfv) U.S. Indication &
Important Safety Information
BOXED WARNING: SERIOUS SKIN REACTIONS
- PADCEV can cause severe and fatal cutaneous adverse reactions
including Stevens-Johnson syndrome (SJS) and Toxic Epidermal
Necrolysis (TEN), which occurred predominantly during the first
cycle of treatment, but may occur later.
- Closely monitor patients for skin reactions.
- Immediately withhold PADCEV and consider referral for
specialized care for suspected SJS or TEN or severe skin
reactions.
- Permanently discontinue PADCEV in patients with confirmed SJS
or TEN; or Grade 4 or recurrent Grade 3 skin reactions.
Indication
PADCEV®, in combination with pembrolizumab, is indicated for the
treatment of adult patients with locally advanced or metastatic
urothelial cancer (mUC).
PADCEV, as a single agent, is indicated for the treatment of
adult patients with locally advanced or mUC who:
- have previously received a programmed death receptor-1 (PD-1)
or programmed death-ligand 1 (PD-L1) inhibitor and
platinum-containing chemotherapy, or
- are ineligible for cisplatin-containing chemotherapy and have
previously received one or more prior lines of therapy.
IMPORTANT SAFETY INFORMATION
Warnings and Precautions
Skin reactions Severe cutaneous adverse reactions,
including fatal cases of SJS or TEN occurred in patients treated
with PADCEV. SJS and TEN occurred predominantly during the first
cycle of treatment but may occur later. Skin reactions occurred in
70% (all grades) of the 564 patients treated with PADCEV in
combination with pembrolizumab in clinical trials. When PADCEV was
given in combination with pembrolizumab, the incidence of skin
reactions, including severe events, occurred at a higher rate
compared to PADCEV as a single agent. The majority of the skin
reactions that occurred with combination therapy included
maculo-papular rash, macular rash and papular rash. Grade 3-4 skin
reactions occurred in 17% of patients (Grade 3: 16%, Grade 4: 1%),
including maculo-papular rash, bullous dermatitis, dermatitis,
exfoliative dermatitis, pemphigoid, rash, erythematous rash,
macular rash, and papular rash. A fatal reaction of bullous
dermatitis occurred in one patient (0.2%). The median time to onset
of severe skin reactions was 1.7 months (range: 0.1 to 17.2
months). Skin reactions led to discontinuation of PADCEV in 6% of
patients.
Skin reactions occurred in 58% (all grades) of the 720 patients
treated with PADCEV as a single agent in clinical trials.
Twenty-three percent (23%) of patients had maculo-papular rash and
34% had pruritus. Grade 3-4 skin reactions occurred in 14% of
patients, including maculo-papular rash, erythematous rash, rash or
drug eruption, symmetrical drug-related intertriginous and flexural
exanthema (SDRIFE), bullous dermatitis, exfoliative dermatitis, and
palmar-plantar erythrodysesthesia. The median time to onset of
severe skin reactions was 0.6 months (range: 0.1 to 8 months).
Among patients experiencing a skin reaction leading to dose
interruption who then restarted PADCEV (n=75), 24% of patients
restarting at the same dose and 24% of patients restarting at a
reduced dose experienced recurrent severe skin reactions. Skin
reactions led to discontinuation of PADCEV in 3.1% of patients.
Monitor patients closely throughout treatment for skin
reactions. Consider topical corticosteroids and antihistamines, as
clinically indicated. For persistent or recurrent Grade 2 skin
reactions, consider withholding PADCEV until Grade ≤1. Withhold
PADCEV and refer for specialized care for suspected SJS, TEN or for
Grade 3 skin reactions. Permanently discontinue PADCEV in patients
with confirmed SJS or TEN; or Grade 4 or recurrent Grade 3 skin
reactions.
Hyperglycemia and diabetic ketoacidosis (DKA), including
fatal events, occurred in patients with and without pre-existing
diabetes mellitus, treated with PADCEV. Patients with baseline
hemoglobin A1C ≥8% were excluded from clinical trials. In clinical
trials of PADCEV as a single agent, 17% of the 720 patients treated
with PADCEV developed hyperglycemia of any grade; 7% of patients
developed Grade 3-4 hyperglycemia (Grade 3: 6.5%, Grade 4: 0.6%).
Fatal events of hyperglycemia and DKA occurred in one patient each
(0.1%). The incidence of Grade 3-4 hyperglycemia increased
consistently in patients with higher body mass index and in
patients with higher baseline A1C. The median time to onset of
hyperglycemia was 0.5 months (range: 0 to 20 months). Hyperglycemia
led to discontinuation of PADCEV in 0.7% of patients. Five percent
(5%) of patients required initiation of insulin therapy for
treatment of hyperglycemia. Of the patients who initiated insulin
therapy for treatment of hyperglycemia, 66% (23/35) discontinued
insulin at the time of last evaluation. Closely monitor blood
glucose levels in patients with, or at risk for, diabetes mellitus
or hyperglycemia. If blood glucose is elevated (>250 mg/dL),
withhold PADCEV.
Pneumonitis/Interstitial Lung Disease (ILD) Severe,
life-threatening or fatal pneumonitis/ILD occurred in patients
treated with PADCEV. When PADCEV was given in combination with
pembrolizumab, 10% of the 564 patients treated with combination
therapy had pneumonitis/ILD of any grade and 4% had Grade 3-4. A
fatal event of pneumonitis/ILD occurred in two patients (0.4%). The
incidence of pneumonitis/ILD, including severe events, occurred at
a higher rate when PADCEV was given in combination with
pembrolizumab compared to PADCEV as a single agent. The median time
to onset of any grade pneumonitis/ILD was 4 months (range: 0.3 to
26 months).
In clinical trials of PADCEV as a single agent, 3% of the 720
patients treated with PADCEV had pneumonitis/ILD of any grade and
0.8% had Grade 3-4. The median time to onset of any grade
pneumonitis/ILD was 2.9 months (range: 0.6 to 6 months).
Monitor patients for signs and symptoms indicative of
pneumonitis/ILD such as hypoxia, cough, dyspnea or interstitial
infiltrates on radiologic exams. Evaluate and exclude infectious,
neoplastic and other causes for such signs and symptoms through
appropriate investigations. Withhold PADCEV for patients who
develop Grade 2 pneumonitis/ILD and consider dose reduction.
Permanently discontinue PADCEV in all patients with Grade 3 or 4
pneumonitis/ILD.
Peripheral neuropathy (PN) When PADCEV was given in
combination with pembrolizumab, 67% of the 564 patients treated
with combination therapy had PN of any grade, 36% had Grade 2
neuropathy, and 7% had Grade 3 neuropathy. The incidence of PN
occurred at a higher rate when PADCEV was given in combination with
pembrolizumab compared to PADCEV as a single agent. The median time
to onset of Grade ≥2 PN was 6 months (range: 0.3 to 25 months).
PN occurred in 53% of the 720 patients treated with PADCEV as a
single agent in clinical trials including 38% with sensory
neuropathy, 8% with muscular weakness and 7% with motor neuropathy.
Thirty percent of patients experienced Grade 2 reactions and 5%
experienced Grade 3-4 reactions. PN occurred in patients treated
with PADCEV with or without preexisting PN. The median time to
onset of Grade ≥2 PN was 4.9 months (range: 0.1 to 20 months).
Neuropathy led to treatment discontinuation in 6% of patients.
Monitor patients for symptoms of new or worsening PN and
consider dose interruption or dose reduction of PADCEV when PN
occurs. Permanently discontinue PADCEV in patients who develop
Grade ≥3 PN.
Ocular disorders were reported in 40% of the 384 patients
treated with PADCEV as a single agent in clinical trials in which
ophthalmologic exams were scheduled. The majority of these events
involved the cornea and included events associated with dry eye
such as keratitis, blurred vision, increased lacrimation,
conjunctivitis, limbal stem cell deficiency, and keratopathy. Dry
eye symptoms occurred in 30% of patients, and blurred vision
occurred in 10% of patients, during treatment with PADCEV. The
median time to onset to symptomatic ocular disorder was 1.7 months
(range: 0 to 30.6 months). Monitor patients for ocular disorders.
Consider artificial tears for prophylaxis of dry eyes and
ophthalmologic evaluation if ocular symptoms occur or do not
resolve. Consider treatment with ophthalmic topical steroids, if
indicated after an ophthalmic exam. Consider dose interruption or
dose reduction of PADCEV for symptomatic ocular disorders.
Infusion site extravasation Skin and soft tissue
reactions secondary to extravasation have been observed after
administration of PADCEV. Of the 720 patients treated with PADCEV
as a single agent in clinical trials, 1% of patients experienced
skin and soft tissue reactions, including 0.3% who experienced
Grade 3-4 reactions. Reactions may be delayed. Erythema, swelling,
increased temperature, and pain worsened until 2-7 days after
extravasation and resolved within 1-4 weeks of peak. Two patients
(0.3%) developed extravasation reactions with secondary cellulitis,
bullae, or exfoliation. Ensure adequate venous access prior to
starting PADCEV and monitor for possible extravasation during
administration. If extravasation occurs, stop the infusion and
monitor for adverse reactions.
Embryo-fetal toxicity PADCEV can cause fetal harm when
administered to a pregnant woman. Advise patients of the potential
risk to the fetus. Advise female patients of reproductive potential
to use effective contraception during PADCEV treatment and for 2
months after the last dose. Advise male patients with female
partners of reproductive potential to use effective contraception
during treatment with PADCEV and for 4 months after the last
dose.
ADVERSE REACTIONS
Most common adverse reactions, including laboratory
abnormalities(≥20%) (PADCEV in combination with pembrolizumab)
Increased aspartate aminotransferase (AST), increased creatinine,
rash, increased glucose, PN, increased lipase, decreased
lymphocytes, increased alanine aminotransferase (ALT), decreased
hemoglobin, fatigue, decreased sodium, decreased phosphate,
decreased albumin, pruritus, diarrhea, alopecia, decreased weight,
decreased appetite, increased urate, decreased neutrophils,
decreased potassium, dry eye, nausea, constipation, increased
potassium, dysgeusia, urinary tract infection and decreased
platelets.
Most common adverse reactions, including laboratory
abnormalities (≥20%) (PADCEV monotherapy) Increased glucose,
increased AST, decreased lymphocytes, increased creatinine, rash,
fatigue, PN, decreased albumin, decreased hemoglobin, alopecia,
decreased appetite, decreased neutrophils, decreased sodium,
increased ALT, decreased phosphate, diarrhea, nausea, pruritus,
increased urate, dry eye, dysgeusia, constipation, increased
lipase, decreased weight, decreased platelets, abdominal pain, dry
skin.
EV-302 Study: 440 patients with previously untreated la/mUC
(PADCEV in combination with pembrolizumab)
Serious adverse reactions occurred in 50% of patients
treated with PADCEV in combination with pembrolizumab. The most
common serious adverse reactions (≥2%) were rash (6%), acute kidney
injury (5%), pneumonitis/ILD (4.5%), urinary tract infection
(3.6%), diarrhea (3.2%), pneumonia (2.3%), pyrexia (2%), and
hyperglycemia (2%). Fatal adverse reactions occurred in 3.9%
of patients treated with PADCEV in combination with pembrolizumab
including acute respiratory failure (0.7%), pneumonia (0.5%), and
pneumonitis/ILD (0.2%).
Adverse reactions leading to discontinuation of PADCEV occurred
in 35% of patients. The most common adverse reactions (≥2%)
leading to discontinuation of PADCEV were PN (15%), rash (4.1%)
and pneumonitis/ILD (2.3%). Adverse reactions leading to dose
interruption of PADCEV occurred in 73% of patients. The most
common adverse reactions (≥2%) leading to dose interruption of
PADCEV were PN (22%), rash (16%), COVID-19 (10%), diarrhea (5%),
pneumonitis/ILD (4.8%), fatigue (3.9%), hyperglycemia (3.6%),
increased ALT (3%) and pruritus (2.5%). Adverse reactions leading
to dose reduction of PADCEV occurred in 42% of patients. The
most common adverse reactions (≥2%) leading to dose reduction
of PADCEV were rash (16%), PN (13%) and fatigue (2.7%).
EV-103 Study: 121 patients with previously untreated la/mUC
who were not eligible for cisplatin-containing chemotherapy (PADCEV
in combination with pembrolizumab)
Serious adverse reactions occurred in 50% of patients
treated with PADCEV in combination with pembrolizumab; the most
common (≥2%) were acute kidney injury (7%), urinary tract infection
(7%), urosepsis (5%), sepsis (3.3%), pneumonia (3.3%), hematuria
(3.3%), pneumonitis/ILD (3.3%), urinary retention (2.5%), diarrhea
(2.5%), myasthenia gravis (2.5%), myositis (2.5%), anemia (2.5%),
and hypotension (2.5%). Fatal adverse reactions occurred in
5% of patients treated with PADCEV in combination with
pembrolizumab, including sepsis (1.6%), bullous dermatitis (0.8%),
myasthenia gravis (0.8%), and pneumonitis/ILD (0.8%). Adverse
reactions leading to discontinuation of PADCEV occurred in 36%
of patients; the most common (≥2%)were PN (20%) and rash (6%).
Adverse reactions leading to dose interruption of PADCEV
occurred in 69% of patients; the most common (≥2%)were PN (18%),
rash (12%), increased lipase (6%), pneumonitis/ILD (6%), diarrhea
(4.1%), acute kidney injury (3.3%), increased ALT (3.3%), fatigue
(3.3%), neutropenia (3.3%), urinary tract infection (3.3%),
increased amylase (2.5%), anemia (2.5%), COVID-19 (2.5%),
hyperglycemia (2.5%), and hypotension (2.5%). Adverse reactions
leading to dose reduction of PADCEV occurred in 45% of
patients; the most common (≥2%) were PN (17%), rash (12%), fatigue
(5%), neutropenia (5%), and diarrhea (4.1%).
EV-301 Study: 296 patients previously treated with a PD-1/L1
inhibitor and platinum-based chemotherapy (PADCEV
monotherapy)
Serious adverse reactions occurred in 47% of patients
treated with PADCEV; the most common (≥2%) were urinary tract
infection, acute kidney injury (7% each), and pneumonia (5%).
Fatal adverse reactions occurred in 3% of patients,
including multiorgan dysfunction (1%), hepatic dysfunction, septic
shock, hyperglycemia, pneumonitis/ILD, and pelvic abscess (0.3%
each). Adverse reactions leading to discontinuation occurred
in 17% of patients; the most common (≥2%) were PN (5%) and rash
(4%). Adverse reactions leading to dose interruption
occurred in 61% of patients; the most common (≥4%) were PN (23%),
rash (11%), and fatigue (9%). Adverse reactions leading to dose
reduction occurred in 34% of patients; the most common (≥2%)
were PN (10%), rash (8%), decreased appetite, and fatigue (3%
each).
EV-201, Cohort 2 Study: 89 patients previously treated with a
PD-1/L1 inhibitor and not eligible for cisplatin-based chemotherapy
(PADCEV monotherapy)
Serious adverse reactions occurred in 39% of patients
treated with PADCEV; the most common (≥3%) were pneumonia, sepsis,
and diarrhea (5% each). Fatal adverse reactions occurred in
8% of patients, including acute kidney injury (2.2%), metabolic
acidosis, sepsis, multiorgan dysfunction, pneumonia, and
pneumonitis/ILD (1.1% each). Adverse reactions leading to
discontinuation occurred in 20% of patients; the most common
(≥2%) was PN (7%). Adverse reactions leading to dose
interruption occurred in 60% of patients; the most common (≥3%)
were PN (19%), rash (9%), fatigue (8%), diarrhea (5%), increased
AST, and hyperglycemia (3% each). Adverse reactions leading to
dose reduction occurred in 49% of patients; the most common
(≥3%) were PN (19%), rash (11%), and fatigue (7%).
DRUG INTERACTIONS
Effects of other drugs on PADCEV (Dual P-gp and Strong
CYP3A4 Inhibitors)
Concomitant use with dual P-gp and strong CYP3A4 inhibitors may
increase unconjugated monomethyl auristatin E exposure, which may
increase the incidence or severity of PADCEV toxicities. Closely
monitor patients for signs of toxicity when PADCEV is given
concomitantly with dual P-gp and strong CYP3A4 inhibitors.
SPECIFIC POPULATIONS
Lactation Advise lactating women not to breastfeed during
treatment with PADCEV and for 3 weeks after the last dose.
Hepatic impairment Avoid the use of PADCEV in patients
with moderate or severe hepatic impairment.
For more information, please see the U.S. full Prescribing
Information including BOXED WARNING for PADCEV
here.
About Pfizer Oncology
At Pfizer Oncology, we are at the forefront of a new era in
cancer care. Our industry-leading portfolio and extensive pipeline
includes three core mechanisms of action to attack cancer from
multiple angles, including small molecules, antibody-drug
conjugates (ADCs), and bispecific antibodies, including other
immune-oncology biologics. We are focused on delivering
transformative therapies in some of the world’s most common
cancers, including breast cancer, genitourinary cancer,
hematology-oncology, and thoracic cancers, which includes lung
cancer. Driven by science, we are committed to accelerating
breakthroughs to help people with cancer live better and longer
lives.
About Astellas
Astellas is a global life sciences company committed to turning
innovative science into VALUE for patients. We provide
transformative therapies in disease areas that include oncology,
ophthalmology, urology, immunology and women's health. Through our
research and development programs, we are pioneering new healthcare
solutions for diseases with high unmet medical need. Learn more at
www.astellas.com.
About the Pfizer, Astellas and Merck Collaboration
Seagen and Astellas entered a clinical collaboration agreement
with Merck to evaluate the combination of Seagen’s and Astellas’
PADCEV® (enfortumab vedotin-ejfv) and Merck’s KEYTRUDA®
(pembrolizumab) in patients with previously untreated metastatic
urothelial cancer. Pfizer Inc. successfully completed its
acquisition of Seagen on December 14, 2023. KEYTRUDA is a
registered trademark of Merck Sharp & Dohme Corp., a subsidiary
of Merck & Co., Inc., Rahway, NJ, USA (known as MSD outside of
the United States and Canada).
Pfizer Disclosure Notice
The information contained in this release is as of February 10,
2025. Pfizer assumes no obligation to update forward-looking
statements contained in this release as the result of new
information or future events or developments.
This release contains forward-looking information about Pfizer
Oncology and PADCEV® (enfortumab vedotin-ejfv) in combination with
pembrolizumab in patients with previously untreated locally
advanced or metastatic urothelial cancer, including their potential
benefits, that involves substantial risks and uncertainties that
could cause actual results to differ materially from those
expressed or implied by such statements. Risk and uncertainties
include, among other things, uncertainties regarding the commercial
success of PADCEV; the uncertainties inherent in research and
development, including the ability to meet anticipated clinical
endpoints, commencement and/or completion dates for our clinical
trials, regulatory submission dates, regulatory approval dates
and/or launch dates, as well as the possibility of unfavorable new
clinical data and further analyses of existing clinical data; the
risk that clinical trial data are subject to differing
interpretations and assessments by regulatory authorities; whether
regulatory authorities will be satisfied with the design of and
results from our clinical studies; whether and when any
applications may be filed in particular jurisdictions for any
potential indication for PADCEV with pembrolizumab or as a single
agent; whether and when any such applications that may be pending
or filed for PADCEV with pembrolizumab or as a single agent may be
approved by regulatory authorities, which will depend on myriad
factors, including making a determination as to whether the
product's benefits outweigh its known risks and determination of
the product's efficacy and, if approved, whether PADCEV with
pembrolizumab or as a single agent will be commercially successful;
decisions by regulatory authorities impacting labeling,
manufacturing processes, safety and/or other matters that could
affect the availability or commercial potential of PADCEV with
pembrolizumab or as a single agent; whether the collaboration
between Pfizer, Astellas and Merck will be successful;
uncertainties regarding the impact of COVID-19 on Pfizer’s
business, operations and financial results; and competitive
developments.
A further description of risks and uncertainties can be found in
Pfizer’s Annual Report on Form 10-K for the fiscal year ended
December 31, 2023, and in its subsequent reports on Form 10-Q,
including in the sections thereof captioned “Risk Factors” and
“Forward-Looking Information and Factors That May Affect Future
Results”, as well as in its subsequent reports on Form 8-K, all of
which are filed with the U.S. Securities and Exchange Commission
and available at www.sec.gov and www.pfizer.com.
Astellas Cautionary Notes
In this press release, statements made with respect to current
plans, estimates, strategies and beliefs and other statements that
are not historical facts are forward-looking statements about the
future performance of Astellas. These statements are based on
management’s current assumptions and beliefs in light of the
information currently available to it and involve known and unknown
risks and uncertainties. A number of factors could cause actual
results to differ materially from those discussed in the
forward-looking statements. Such factors include, but are not
limited to: (i) changes in general economic conditions and in laws
and regulations, relating to pharmaceutical markets, (ii) currency
exchange rate fluctuations, (iii) delays in new product launches,
(iv) the inability of Astellas to market existing and new products
effectively, (v) the inability of Astellas to continue to
effectively research and develop products accepted by customers in
highly competitive markets, and (vi) infringements of Astellas’
intellectual property rights by third parties. Information about
pharmaceutical products (including products currently in
development) which is included in this press release is not
intended to constitute an advertisement or medical advice.
+++
References
1 Powels T, et al. EV-302: Updated analysis from the phase 3
global study of enfortumab vedotin in combination with
pembrolizumab (EV+P) vs chemotherapy (chemo) in previously
untreated locally advanced or metastatic urothelial carcinoma
(la/mUC). J Clin Oncol 43, 2025 (suppl 5; abstr 664) 2 Powels T,
Valderrama BP, Gupta S, et al. Enfortumab Vedotin and Pembrolizumab
in Untreated Advanced Urothelial Cancer. N Engl J Med
2024;390:875-888. 3 PADCEV [package insert]. Northbrook, IL:
Astellas Pharma US, Inc. 4 National Cancer Institute. Enfortumab
Vedotin and Pembrolizumab vs Chemotherapy Alone in Untreated
Locally Advanced or Metastatic Urothelial Cancer (EV-302).
ClinicalTrials.gov identifier: NCT04223856. Published January 6,
2020. Updated September 27, 2024. Accessed January 6, 2025.
https://clinicaltrials.gov/study/NCT04223856?tab=results#results-overview.
5 Challita-Eid PM, Satpayev D, Yang P, et al. Enfortumab vedotin
antibody-drug conjugate targeting nectin-4 is a highly potent
therapeutic agent in multiple preclinical cancer models. Cancer Res
2016;76(10):3003-13.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20250210184062/en/
Pfizer Contacts: +1-212-733-1226
PfizerMediaRelations@Pfizer.com
For Investors +1-212-733-4848 IR@pfizer.com
Astellas Contacts: Tara Grayczyk +1-847-686-1813
Tara.Grayczyk@Astellas.com
Corporate Communications +81-3-3244-3202
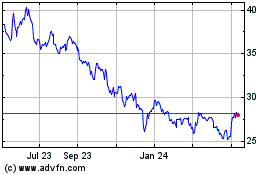
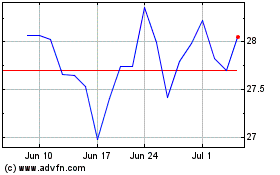
Pfizer (NYSE:PFE)
Historical Stock Chart
From Jan 2025 to Feb 2025
Pfizer (NYSE:PFE)
Historical Stock Chart
From Feb 2024 to Feb 2025