- Two oral presentations and five poster presentations at ASH
Annual Meeting exhibit new and updated data in the clinical
development program for ciltacabtagene autoleucel (cilta-cel)
- Patient-reported outcomes (PROs) from the CARTITUDE-4 study of
cilta-cel versus standard of care in patients with
lenalidomide-refractory multiple myeloma after one to three lines
of therapy will be presented
- Updated data from Cohorts A and B of the CARTITUDE-2 study
evaluating the safety and efficacy of cilta-cel in patients with
multiple myeloma and 1-3 prior lines of therapy (Cohort A) and with
early relapse after first line treatment (Cohort B) will also be
highlighted at the meeting
Legend Biotech Corporation (“Legend Biotech” or the “Company”)
(NASDAQ: LEGN), a global biotechnology company developing,
manufacturing and commercializing novel therapies to treat
life-threatening diseases, today announced that two oral
presentations and five poster presentations featuring new and
updated data from the CARTITUDE clinical development program
evaluating ciltacabtagene autoleucel (cilta-cel) will be presented
at the 65th American Society of Hematology Annual Meeting and
Exposition taking place in San Diego from December 9-12.
For the first time, patient reported outcomes from the Phase 3
CARTITUDE-4 study of cilta-cel versus standard of care treatment in
patients with lenalidomide-refractory multiple myeloma after one to
three prior lines of therapy will be featured in an oral
presentation at ASH. A poster will also present a new analysis of
the CARTITUDE-4 study evaluating the efficacy and safety in
patients who received cilta-cel as study treatment.
“We continue to deepen our understanding of the safety and
efficacy profile for cilta-cel in different patient populations and
in earlier lines of treatment in the CARTITUDE clinical development
program,” said Ying Huang, Ph.D., Chief Executive Officer of Legend
Biotech. “We remain steadfast in our commitment to deliver
additional treatment options to patients with unmet needs and are
pleased with the results of our data. We look forward to seeing the
latest data presented during ASH.”
A second oral presentation will include updated efficacy and
safety data from Cohorts A and B of the Phase 2 CARTITUDE-2 study
evaluating treatment with cilta-cel for patients with relapsed or
refractory multiple myeloma who have received one to three prior
lines of treatment or with early relapse after first-time
treatment.
Oral and poster presentation abstracts from the meeting can be
found below.
ASH Presentations (December 9-12, 2023)
Abstract Number
Title
Information
Abstract #1021
Oral Presentation
The Phase 2 CARTITUDE-2 Trial: Updated
Efficacy and Safety of Ciltacabtagene Autoleucel in Patients with
Multiple Myeloma and 1–3 Prior Lines of Therapy (Cohort A) and With
Early Relapse After First Line Treatment (Cohort B)
Session Name: 704. Cellular
Immunotherapies: Early Phase and Investigational Therapies: CAR-T
Cell Therapies for Multiple Myeloma and B Cell Lymphomas
Session Date/Time: December 11,
2023, 4:30 pm – 6:00 pm PT
Presentation Date/Time: December
11, 2023, 4:30 pm PT
Location: San Diego Convention
Center, Room 6A
Abstract #1063
Oral Presentation
Patient-Reported Outcomes in the Phase 3
CARTITUDE-4 Study of Ciltacabtagene Autoleucel Versus Standard of
Care in Patients With Lenalidomide-Refractory Multiple Myeloma
After 1–3 Lines of Therapy
Session Name: 905. Outcomes
Research – Lymphoid Malignancies: Balancing Efficacy, Safety and
Tolerability, and Quality of Life in Patients With Multiple
Myeloma
Session Date/Time: December 11,
2023, 4:30 pm – 6:00 pm PT
Presentation Date/Time: December
11, 2023, 4:30 pm PT
Location: Marriott Marquis San
Diego Marina, Marriott Grand Ballroom 2-4
Abstract #2099
Poster Presentation
Biomarker Correlates of Response to
Ciltacabtagene Autoleucel in Patients With Relapsed or Refractory
Multiple Myeloma From CARTITUDE-1, a Phase 1b/2 Open-label Study,
at the ~3 Year Follow-up
Session Name: 704. Cellular
Immunotherapies: Early Phase and Investigational Therapies: Poster
I
Session Date/Time: December 9,
2023, 5:30 - 7:30 pm PT
Location: San Diego Convention
Center, Halls G-H
Abstract #2141
Poster Presentation
Comparative Efficacy of Ciltacabtagene
Autoleucel Versus Idecabtagene Vicleucel in the Treatment of
Patients With Relapsed or Refractory Multiple Myeloma Previously
Treated With 2–4 Prior Lines of Therapy Using A Matching-Adjusted
Indirect Comparison
Session Name: 705. Cellular
Immunotherapies: Late Phase and Commercially Available Therapies:
Poster I
Session Date/Time: December 9,
2023, 5:30 - 7:30 pm PT
Location: San Diego Convention
Center, Halls G-H
Abstract #3501
Poster Presentation
Clinical Experience with Cranial Nerve
Impairment in the CARTITUDE-1, CARTITUDE-2 Cohorts A, B and C, and
CARTITUDE-4 Studies of Ciltacabtagene Autoleucel (cilta-cel)
Session Name: 705. Cellular
Immunotherapies: Late Phase and Commercially Available Therapies:
Poster II
Session Date/Time: December 10,
2023, 6:00 - 8:00 pm PT
Location: San Diego Convention
Center, Halls G-H
Abstract #4866
Poster Presentation
Efficacy and Safety in Patients With
Lenalidomide-Refractory Multiple Myeloma and 1-3 Prior Lines Who
Received a Single Infusion of Ciltacabtagene Autoleucel As Study
Treatment in the Phase 3 CARTITUDE-4 Trial
Session Name: 705. Cellular
Immunotherapies: Late Phase and Commercially Available Therapies:
Poster III
Session Date/Time: December 11,
2023, 6:00 - 8:00 pm PT
Location: San Diego Convention
Center, Halls G-H
Abstract #5083
Poster Presentation
Cost per Responder Analysis of Patients
With Lenalidomide-Refractory Multiple Myeloma Who Received
Cilta-cel From the CARTITUDE-4 Trial
Session Name: 902. Health Services
and Quality Improvement – Lymphoid Malignancies: Poster III
Session Date/Time: December 11,
2023, 6:00 – 8:00 pm PT
Location: San Diego Convention
Center, Halls G-H
ABOUT CARVYKTI® (CILTACABTAGENE AUTOLEUCEL;
CILTA-CEL)
Ciltacabtagene autoleucel is a B-cell maturation antigen
(BCMA)-directed, genetically modified autologous T-cell
immunotherapy, which involves reprogramming a patient’s own T-cells
with a transgene encoding a chimeric antigen receptor (CAR) that
identifies and eliminates cells that express BCMA. BCMA is
primarily expressed on the surface of malignant multiple myeloma
B-lineage cells, as well as late-stage B-cells and plasma cells.
The cilta-cel CAR protein features two BCMA-targeting single domain
antibodies designed to confer high avidity against human BCMA. Upon
binding to BCMA-expressing cells, the CAR promotes T-cell
activation, expansion, and elimination of target cells.1
In December 2017, Legend Biotech entered into an exclusive
worldwide license and collaboration agreement with Janssen Biotech,
Inc. (Janssen) to develop and commercialize cilta-cel.
ABOUT CARTITUDE-1
CARTITUDE-1 (NCT03548207) is a Phase 1b/2, open-label, single
arm, multi-center trial evaluating cilta-cel for the treatment of
adult patients with relapsed or refractory multiple myeloma, who
previously received at least three prior lines of therapy including
a proteasome inhibitor (PI), an immunomodulatory drug (IMiD) and an
anti-CD38 monoclonal antibody. The primary objective of the Phase
1b portion of the study was to characterize the safety and confirm
the recommended Phase 2 dose of cilta-cel. The Phase 2 portion
further evaluated the efficacy of cilta-cel with overall response
rate as the primary endpoint.2
ABOUT CARTITUDE-2
CARTITUDE-2 (NCT04133636) is an ongoing Phase 2 multicohort
study evaluating the safety and efficacy of cilta-cel in various
clinical settings (Cohorts A, B, C, D, E, F). The primary study
objective is to measure the percentage of patients with negative
minimal residual disease (MRD).3
ABOUT CARTITUDE-4
CARTITUDE-4 (NCT04181827) is an ongoing, international,
randomized, open-label Phase 3 study evaluating the efficacy and
safety of cilta-cel versus pomalidomide, bortezomib and
dexamethasone (PVd) or daratumumab, pomalidomide and dexamethasone
(DPd) in adult patients with relapsed and lenalidomide-refractory
multiple myeloma who received one to three prior lines of therapy,
including a PI and an IMiD. The primary endpoint of the study was
progression-free survival.4
ABOUT MULTIPLE MYELOMA
Multiple myeloma is an incurable blood cancer that starts in the
bone marrow and is characterized by an excessive proliferation of
plasma cells.5 In 2023, it is estimated that more than 35,000
people will be diagnosed with multiple myeloma, and more than
12,000 people will die from the disease in the U.S.6 While some
patients with multiple myeloma initially have no symptoms, most
patients are diagnosed due to symptoms that can include bone
problems, low blood counts, calcium elevation, kidney problems or
infections.7
CARVYKTI® INDICATIONS AND USAGE
CARVYKTI® (ciltacabtagene autoleucel) is a B-cell maturation
antigen (BCMA)-directed genetically modified autologous T cell
immunotherapy indicated for the treatment of adult patients with
relapsed or refractory multiple myeloma, after four or more prior
lines of therapy, including a proteasome inhibitor, an
immunomodulatory agent, and an anti-CD38 monoclonal antibody.
CARVYKTI® IMPORTANT SAFETY INFORMATION
WARNING: CYTOKINE RELEASE SYNDROME,
NEUROLOGIC TOXICITIES, HLH/MAS, and PROLONGED and RECURRENT
CYTOPENIA Cytokine Release Syndrome (CRS), including fatal
or life-threatening reactions, occurred in patients following
treatment with CARVYKTI®. Do not administer CARVYKTI® to patients
with active infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids. Immune Effector Cell-Associated
Neurotoxicity Syndrome (ICANS), which may be fatal or
life-threatening, occurred following treatment with CARVYKTI®,
including before CRS onset, concurrently with CRS, after CRS
resolution, or in the absence of CRS. Monitor for neurologic events
after treatment with CARVYKTI®. Provide supportive care and/or
corticosteroids as needed. Parkinsonism and Guillain-Barré
syndrome and their associated complications resulting in fatal or
life-threatening reactions have occurred following treatment with
CARVYKTI®. Hemophagocytic Lymphohistiocytosis/Macrophage
Activation Syndrome (HLH/MAS), including fatal and life-threatening
reactions, occurred in patients following treatment with CARVYKTI®.
HLH/MAS can occur with CRS or neurologic toxicities.
Prolonged and/or recurrent cytopenias with bleeding and
infection and requirement for stem cell transplantation for
hematopoietic recovery occurred following treatment with CARVYKTI®.
CARVYKTI® is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
CARVYKTI® REMS Program.
WARNINGS AND PRECAUTIONS
Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred following treatment with
CARVYKTI® in 95% (92/97) of patients receiving ciltacabtagene
autoleucel. Grade 3 or higher CRS (2019 ASTCT grade) occurred in 5%
(5/97) of patients, with Grade 5 CRS reported in 1 patient. The
median time to onset of CRS was 7 days (range: 112 days). The most
common manifestations of CRS included pyrexia (100%), hypotension
(43%), increased aspartate aminotransferase (AST) (22%), chills
(15%), increased alanine aminotransferase (ALT) (14%) and sinus
tachycardia (11%). Grade 3 or higher events associated with CRS
included increased AST and ALT, hyperbilirubinemia, hypotension,
pyrexia, hypoxia, respiratory failure, acute kidney injury,
disseminated intravascular coagulation and hemorrhage, HLH/MAS,
angina pectoris, supraventricular and ventricular tachycardia,
malaise, myalgias, increased Creactive protein, ferritin, blood
alkaline phosphatase and gamma-glutamyl transferase.
Identify CRS based on clinical presentation. Evaluate for and
treat other causes of fever, hypoxia and hypotension. CRS has been
reported to be associated with findings of HLH/MAS, and the
physiology of the syndromes may overlap. HLH/MAS is a potentially
life-threatening condition. In patients with progressive symptoms
of CRS or refractory CRS despite treatment, evaluate for evidence
of HLH/MAS. One patient with CRS and suspected HLH/MAS developed a
fatal retroperitoneal hemorrhage in the setting of
thrombocytopenia, coagulopathy and anticoagulation.
Sixty-nine of 97 (71%) patients received tocilizumab and/or a
corticosteroid for CRS after infusion of ciltacabtagene autoleucel.
Forty-four (45%) patients received only tocilizumab, of whom 33
(34%) received a single dose and 11 (11%) received more than one
dose; 24 patients (25%) received tocilizumab and a corticosteroid,
and one patient (1%) received only corticosteroids. Ensure that a
minimum of two doses of tocilizumab are available prior to infusion
of CARVYKTI®.
Monitor patients at least daily for 10 days following CARVYKTI®
infusion at a REMS-certified healthcare facility for signs and
symptoms of CRS. Monitor patients for signs or symptoms of CRS for
at least 4 weeks after infusion. At the first sign of CRS,
immediately institute treatment with supportive care, tocilizumab,
or tocilizumab and corticosteroids.
Counsel patients to seek immediate medical attention should
signs or symptoms of CRS occur at any time.
Neurologic toxicities, which may be severe,
life-threatening or fatal, occurred following treatment with
CARVYKTI®. Neurologic toxicities included ICANS, neurologic
toxicity with signs and symptoms of parkinsonism, Guillain-Barré
Syndrome, immune mediated myelitis, peripheral neuropathies, and
cranial nerve palsies. Counsel patients on the signs and symptoms
of these neurologic toxicities, and on the delayed nature of onset
of some of these toxicities. Instruct patients to seek immediate
medical attention for further assessment and management if signs or
symptoms of any of these neurologic toxicities occur at any
time.
Overall, one or more subtypes of neurologic toxicity described
below occurred following ciltacabtagene autoleucel in 26% (25/97)
of patients, of which 11% (11/97) of patients experienced Grade 3
or higher events. These subtypes of neurologic toxicities were also
observed in two ongoing studies.
Immune Effector Cell-Associated
Neurotoxicity Syndrome (ICANS): Patients may experience
fatal or life-threatening ICANS following treatment with CARVYKTI®,
including before CRS onset, concurrently with CRS, after CRS
resolution, or in the absence of CRS. ICANS occurred in 23% (22/97)
of patients receiving ciltacabtagene autoleucel including Grade 3
or 4 events in 3% (3/97) and Grade 5 (fatal) events in 2% (2/97).
The median time to onset of ICANS was 8 days (range 1-28 days). All
22 patients with ICANS had CRS. The most frequent (≥5%)
manifestation of ICANS included encephalopathy (23%), aphasia (8%)
and headache (6%).
Monitor patients at least daily for 10 days following CARVYKTI®
infusion at the REMS-certified healthcare facility for signs and
symptoms of ICANS. Rule out other causes of ICANS symptoms. Monitor
patients for signs or symptoms of ICANS for at least 4 weeks after
infusion and treat promptly. Neurologic toxicity should be managed
with supportive care and/or corticosteroids as needed.
Parkinsonism: Of the 25 patients in
the CARTITUDE-1 study experiencing any neurotoxicity, five male
patients had neurologic toxicity with several signs and symptoms of
parkinsonism, distinct from immune effector cell-associated
neurotoxicity syndrome (ICANS). Neurologic toxicity with
parkinsonism has been reported in other ongoing trials of
ciltacabtagene autoleucel. Patients had parkinsonian and
non-parkinsonian symptoms that included tremor, bradykinesia,
involuntary movements, stereotypy, loss of spontaneous movements,
masked facies, apathy, flat affect, fatigue, rigidity, psychomotor
retardation, micrographia, dysgraphia, apraxia, lethargy,
confusion, somnolence, loss of consciousness, delayed reflexes,
hyperreflexia, memory loss, difficulty swallowing, bowel
incontinence, falls, stooped posture, shuffling gait, muscle
weakness and wasting, motor dysfunction, motor and sensory loss,
akinetic mutism, and frontal lobe release signs. The median onset
of parkinsonism in the 5 patients in CARTITUDE-1 was 43 days (range
15-108) from infusion of ciltacabtagene autoleucel.
Monitor patients for signs and symptoms of parkinsonism that may
be delayed in onset and managed with supportive care measures.
There is limited efficacy information with medications used for the
treatment of Parkinson’s disease, for the improvement or resolution
of parkinsonism symptoms following CARVYKTI® treatment.
Guillain-Barré Syndrome: A fatal
outcome following Guillain-Barré Syndrome (GBS) has occurred in
another ongoing study of ciltacabtagene autoleucel despite
treatment with intravenous immunoglobulins. Symptoms reported
include those consistent with Miller-Fisher variant of GBS,
encephalopathy, motor weakness, speech disturbances and
polyradiculoneuritis.
Monitor for GBS. Evaluate patients presenting with peripheral
neuropathy for GBS. Consider treatment of GBS with supportive care
measures and in conjunction with immunoglobulins and plasma
exchange, depending on severity of GBS.
Immune Mediated Myelitis: Grade 3
myelitis has occurred 25 days following treatment in another
ongoing study. Symptoms reported included hypoesthesia of the lower
extremities and the lower abdomen with impaired sphincter control.
Symptoms improved with the use of corticosteroids and intravenous
immune globulin. Myelitis was ongoing at the time of death from
other cause.
Peripheral Neuropathy: Six patients
in CARTITUDE-1 developed peripheral neuropathy. These neuropathies
presented as sensory, motor or sensorimotor neuropathies. Median
time of onset of symptoms was 62 days (range 4-136 days), median
duration of peripheral neuropathies was 256 days (range 2-465 days)
including those with ongoing neuropathy. Patients who experienced
peripheral neuropathy also experienced cranial nerve palsies or GBS
in other ongoing trials of ciltacabtagene autoleucel. Monitor
patients for signs and symptoms of peripheral neuropathies.
Cranial Nerve Palsies: Three
patients (3.1%) experienced cranial nerve palsies in CARTITUDE-1.
All three patients had 7th cranial nerve palsy; one patient had 5th
cranial nerve palsy as well. Median time to onset was 26 days
(range 21-101 days) following infusion of ciltacabtagene
autoleucel. Occurrence of 3rd and 6th cranial nerve palsy,
bilateral 7th cranial nerve palsy, worsening of cranial nerve palsy
after improvement, and occurrence of peripheral neuropathy in
patients with cranial nerve palsy have also been reported in
ongoing trials of ciltacabtagene autoleucel. Monitor patients for
signs and symptoms of cranial nerve palsies. Consider management
with systemic corticosteroids, depending on the severity and
progression of signs and symptoms.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage
Activation Syndrome (MAS): Fatal HLH occurred in one patient
(1%), 99 days after ciltacabtagene autoleucel. The HLH event was
preceded by prolonged CRS lasting 97 days. The manifestations of
HLH/MAS include hypotension, hypoxia with diffuse alveolar damage,
coagulopathy, cytopenia, and multi-organ dysfunction, including
renal dysfunction.
One patient with grade 4 HLH/MAS developed fatal intracerebral
and gastrointestinal hemorrhage in the setting of coagulopathy and
thrombocytopenia 12 days after treatment in another ongoing study.
Patients who develop HLH/MAS have an increased risk of severe
bleeding. Monitor hematological parameters in patients with HLH/MAS
and transfuse per institutional guidelines.
HLH is a life-threatening condition with a high mortality rate
if not recognized and treated early. Treatment of HLH/MAS should be
administered per institutional standards.
CARVYKTI® REMS: Because of the risk of CRS and neurologic
toxicities, CARVYKTI® is available only through a restricted
program under a Risk Evaluation and Mitigation Strategy (REMS)
called the CARVYKTI® REMS.
Further information is available at
https://www.carvyktirems.com/ or 1-844-672-0067.
Prolonged and Recurrent Cytopenias: Patients may exhibit
prolonged and recurrent cytopenias following lymphodepleting
chemotherapy and CARVYKTI® infusion. One patient underwent
autologous stem cell therapy for hematopoietic reconstitution due
to prolonged thrombocytopenia.
In CARTITUDE-1, 30% (29/97) of patients experienced prolonged
Grade 3 or 4 neutropenia and 41% (40/97) of patients experienced
prolonged Grade 3 or 4 thrombocytopenia that had not resolved by
Day 30 following ciltacabtagene autoleucel infusion.
Recurrent Grade 3 or 4 neutropenia, thrombocytopenia,
lymphopenia and anemia were seen in 63% (61/97), 18% (17/97), 60%
(58/97), and 37% (36/97) after recovery from initial Grade 3 or 4
cytopenia following infusion. After Day 60 following ciltacabtagene
autoleucel infusion, 31%, 12% and 6% of patients had a recurrence
of Grade 3 or higher lymphopenia, neutropenia and thrombocytopenia,
respectively, after initial recovery of their Grade 3 or 4
cytopenia. Eighty-seven percent (84/97) of patients had one, two,
or three or more recurrences of Grade 3 or 4 cytopenias after
initial recovery of Grade 3 or 4 cytopenia. Six and 11 patients had
Grade 3 or 4 neutropenia and thrombocytopenia, respectively, at the
time of death.
Monitor blood counts prior to and after CARVYKTI® infusion.
Manage cytopenias with growth factors and blood product transfusion
support according to local institutional guidelines.
Infections: CARVYKTI® should not be administered to
patients with active infection or inflammatory disorders. Severe,
life-threatening or fatal infections occurred in patients after
CARVYKTI® infusion.
Infections (all grades) occurred in 57 (59%) patients. Grade 3
or 4 infections occurred in 23% (22/97) of patients; Grade 3 or 4
infections with an unspecified pathogen occurred in 17%, viral
infections in 7%, bacterial infections in 1%, and fungal infections
in 1% of patients. Overall, four patients had Grade 5 infections:
lung abscess (n=1), sepsis (n=2) and pneumonia (n=1).
Grade 5 infections reported in other studies include
bronchopulmonary aspergillosis, pneumocystis jirovecii pneumonia,
and CMV colitis (with HSV-1 hepatitis). Another patient developed
mycotic aneurysm due to cerebral aspergillosis and died of
subarachnoid hemorrhage.
Monitor patients for signs and symptoms of infection before and
after CARVYKTI® infusion and treat patients appropriately.
Administer prophylactic, pre-emptive and/or therapeutic
antimicrobials according to the standard institutional guidelines.
Febrile neutropenia was observed in 10% of patients after
ciltacabtagene autoleucel infusion and may be concurrent with CRS.
In the event of febrile neutropenia, evaluate for infection and
manage with broad-spectrum antibiotics, fluids and other supportive
care, as medically indicated.
In a randomized controlled study of relapsed or refractory
multiple myeloma (CARTITUDE- 4), patients treated with
ciltacabtagene autoleucel had an increased rate of fatal COVID-19
infections compared to the standard therapy arm. Counsel patients
on the importance of prevention measures. Follow institutional
guidelines for the vaccination and management of immunocompromised
patients with COVID-19.
Viral Reactivation: Hepatitis B
virus (HBV) reactivation, in some cases resulting in fulminant
hepatitis, hepatic failure and death, can occur in patients with
hypogammaglobulinemia. Perform screening for Cytomegalovirus (CMV),
HBV, hepatitis C virus (HCV), and human immunodeficiency virus
(HIV), or any other infectious agents if clinically indicated in
accordance with clinical guidelines before collection of cells for
manufacturing. Consider antiviral therapy to prevent viral
reactivation per local institutional guidelines/clinical
practice.
Hypogammaglobulinemia was reported as an adverse event in
12% (12/97) of patients; laboratory IgG levels fell below 500 mg/dL
after infusion in 92% (89/97) of patients. Monitor immunoglobulin
levels after treatment with CARVYKTI® and administer IVIG for IgG
<400 mg/dL. Manage per local institutional guidelines, including
infection precautions and antibiotic or antiviral prophylaxis.
Use of Live Vaccines: The safety of
immunization with live viral vaccines during or following CARVYKTI®
treatment has not been studied. Vaccination with live virus
vaccines is not recommended for at least 6 weeks prior to the start
of lymphodepleting chemotherapy, during CARVYKTI® treatment and
until immune recovery following treatment with CARVYKTI®.
Hypersensitivity Reactions have occurred in 5% (5/97) of
patients following ciltacabtagene autoleucel infusion. Serious
hypersensitivity reactions, including anaphylaxis, may be due to
the dimethyl sulfoxide (DMSO) in CARVYKTI®. Patients should be
carefully monitored for 2 hours after infusion for signs and
symptoms of severe reaction. Treat promptly and manage
appropriately according to the severity of the hypersensitivity
reaction.
Secondary Malignancies: Patients may develop secondary
malignancies. Monitor life-long for secondary malignancies. In the
event that a secondary malignancy occurs, contact Janssen Biotech,
Inc., at 1-800-526-7736 for reporting and to obtain instructions on
collection of patient samples for testing of secondary malignancy
of T cell origin.
Effects on Ability to Drive and Use Machines: Due to the
potential for neurologic events, including altered mental status,
seizures, neurocognitive decline, or neuropathy, patients are at
risk for altered or decreased consciousness or coordination in the
8 weeks following CARVYKTI® infusion. Advise patients to refrain
from driving and engaging in hazardous occupations or activities,
such as operating heavy or potentially dangerous machinery during
this initial period, and in the event of new onset of any
neurologic toxicities.
ADVERSE REACTIONS
The most common non-laboratory adverse reactions (incidence
greater than 20%) are pyrexia, cytokine release syndrome,
hypogammaglobulinemia, hypotension, musculoskeletal pain, fatigue,
infections of unspecified pathogen, cough, chills, diarrhea,
nausea, encephalopathy, decreased appetite, upper respiratory tract
infection, headache, tachycardia, dizziness, dyspnea, edema, viral
infections, coagulopathy, constipation and vomiting. The most
common laboratory adverse reactions (incidence greater than or
equal to 50%) include thrombocytopenia, neutropenia, anemia,
aminotransferase elevation and hypoalbuminemia.
Please read full Prescribing Information including Boxed Warning
for CARVYKTI®.
ABOUT LEGEND BIOTECH
Legend Biotech is a global biotechnology company dedicated to
treating, and one day curing, life-threatening diseases.
Headquartered in Somerset, New Jersey, we are developing advanced
cell therapies across a diverse array of technology platforms,
including autologous and allogeneic chimeric antigen receptor
T-cell, gamma-delta T cell (gd T) and natural killer (NK)
cell-based immunotherapy. From our three R&D sites around the
world, we apply these innovative technologies to pursue the
discovery of cutting-edge therapeutics for patients worldwide.
Learn more at www.legendbiotech.com and follow us on Twitter and
LinkedIn.
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
Statements in this press release about future expectations,
plans and prospects, as well as any other statements regarding
matters that are not historical facts, constitute “forward-looking
statements” within the meaning of The Private Securities Litigation
Reform Act of 1995. These statements include, but are not limited
to, statements relating to Legend Biotech’s expectations for
CARVYKTI®, such as Legend Biotech’s manufacturing and
commercialization expectations for CARVYKTI® and the potential
effect of treatment with CARVYKTI®, and the potential benefits of
Legend Biotech’s product candidates. The words “anticipate,”
“believe,” “continue,” “could,” “estimate,” “expect,” “intend,”
“may,” “plan,” “potential,” “predict,” “project,” “should,”
“target,” “will,” “would” and similar expressions are intended to
identify forward-looking statements, although not all
forward-looking statements contain these identifying words. Actual
results may differ materially from those indicated by such
forward-looking statements as a result of various important
factors. Legend Biotech’s expectations could be affected by, among
other things, uncertainties involved in the development of new
pharmaceutical products; unexpected clinical trial results,
including as a result of additional analysis of existing clinical
data or unexpected new clinical data; unexpected regulatory actions
or delays, including requests for additional safety and/or efficacy
data or analysis of data, or government regulation generally;
unexpected delays as a result of actions undertaken, or failures to
act, by our third party partners; uncertainties arising from
challenges to Legend Biotech’s patent or other proprietary
intellectual property protection, including the uncertainties
involved in the U.S. litigation process; competition in general;
government, industry, and general product pricing and other
political pressures; the duration and severity of the COVID-19
pandemic and governmental and regulatory measures implemented in
response to the evolving situation; as well as the other factors
discussed in the “Risk Factors” section of Legend Biotech’s Annual
Report on Form 20-F filed with the Securities and Exchange
Commission on March 30, 2023. Should one or more of these risks or
uncertainties materialize, or should underlying assumptions prove
incorrect, actual results may vary materially from those described
in this press release as anticipated, believed, estimated or
expected. Any forward-looking statements contained in this press
release speak only as of the date of this press release. Legend
Biotech specifically disclaims any obligation to update any
forward-looking statement, whether as a result of new information,
future events or otherwise.
1 CARVYKTI Prescribing Information. Horsham, PA: Janssen
Biotech, Inc.
2 ClinicalTrials.gov. A Study of JNJ-68284528, a Chimeric
Antigen Receptor T Cell (CAR-T) Therapy Directed Against B-Cell
Maturation Antigen (BCMA) in Participants With Relapsed or
Refractory Multiple Myeloma (CARTITUDE-1). Available at:
https://clinicaltrials.gov/study/NCT03548207. Last accessed Nov
2023.
3 ClinicalTrials.gov. A Study of JNJ-68284528, a Chimeric
Antigen Receptor T Cell (CAR-T) Therapy Directed Against B-cell
Maturation Antigen (BCMA) in Participants With Multiple Myeloma
(CARTITUDE-2). Available at:
https://clinicaltrials.gov/study/NCT04133636. Last accessed Nov
2023.
4 ClinicalTrials.gov. A Study Comparing JNJ-68284528, a CAR-T
Therapy Directed Against B-cell Maturation Antigen (BCMA), Versus
Pomalidomide, Bortezomib and Dexamethasone (PVd) or Daratumumab,
Pomalidomide and Dexamethasone (DPd) in Participants With Relapsed
and Lenalidomide-Refractory Multiple Myeloma (CARTITUDE-4).
Available at: https://clinicaltrials.gov/study/NCT04181827. Last
accessed Nov 2023.
5 American Society of Clinical Oncology. Multiple myeloma:
introduction.
https://www.cancer.net/cancer-types/multiple-myeloma/introduction.
Accessed October 2023.
6 American Cancer Society. “Key Statistics About Multiple
Myeloma.” Available at:
https://www.cancer.org/cancer/multiple-myeloma/about/key-statistics.html#:~:text=Multiple%20myeloma%20is%20a%20relatively,men%20and%2015%2C370%20in%20women).
Accessed Nov 2023.
7 American Cancer Society. Multiple myeloma: early detection,
diagnosis and staging. Available at:
https://www.cancer.org/content/dam/CRC/PDF/Public/8740.00.pdf.
Accessed Nov 2023.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20231101300547/en/
PRESS CONTACT: Tina Carter, Corporate Communications
Lead, Legend Biotech tina.carter@legendbiotech.com (908)
331-5025
INVESTOR CONTACTS: Jessie Yeung, Head of Investor
Relations and Public Relations, Legend Biotech
jessie.yeung@legendbiotech.com
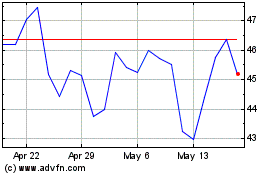
Legend Biotech (NASDAQ:LEGN)
Historical Stock Chart
From Nov 2024 to Dec 2024
Legend Biotech (NASDAQ:LEGN)
Historical Stock Chart
From Dec 2023 to Dec 2024


